Carotid and Vertebral Artery Stenting
Why is carotid artery or vertebral artery stenting required?
The carotid and vertebral arteries are four major blood vessels that supply blood to the brain. The carotid arteries are located in the front of the neck – one on each side and the vertebral arteries are located at the back of neck which also has one on each side of the neck.
Overtime a fatty material called plaque (known as atherosclerosis) can build up in the artery: This may then cause narrowing or blockage to the carotid or vertebral arteries and reduce the blood supply to the brain. This build up of plaque can increase the risk of mini-strokes (Transient Ischaemic Attack - TIA) or major strokes.
Treatment to open the artery is offered to reduce the risk of a stroke in the future.
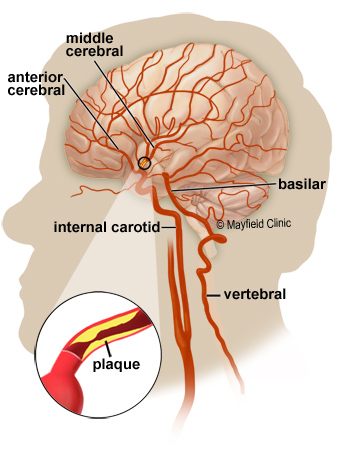
(Picture from google images mayfieldclinic.com)
What is a stent?
Carotid or vertebral artery stenting is an endovascular treatment which means it is performed through a blood vessel by a consultant interventional neuro-radiologist. The procedure is usually carried out under local anaesthetic.
A stent is a tubular structure made with a highly precise metal mesh. Stents are usually made of nitinol (nickel and titanium alloy) or cobalt-chromium (cobalt and chromium alloy). They vary in length and diameter.
The stent is a permanent implant that opens up blocked or narrowed arteries which allows improved blood flow to the brain.
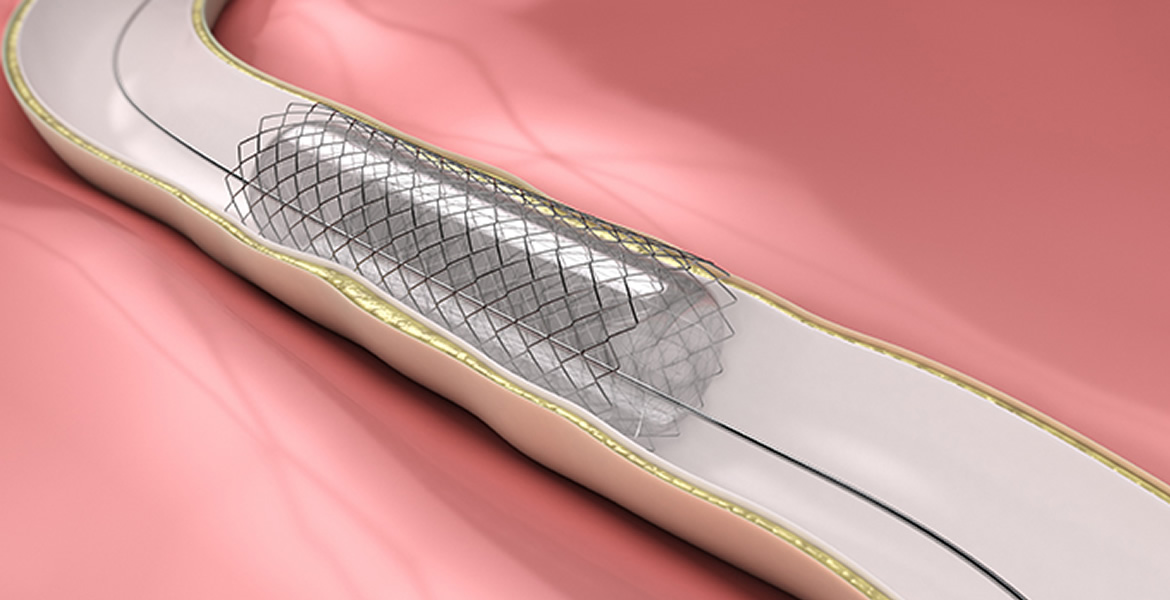
(Picture from google images pvasatx.com)
What happens before the procedure?
You are generally brought to pre op clinic to be assessed and allow you to ask questions regarding the procedure. If your procedure is deemed to be more urgent then you will be brought straight to the ward and seen by a doctor there.
The pre op clinic visit usually lasts up to 2 hours as a detailed clinical history and examination takes place and tests completed to ensure your safety.
You should drink about 2 litres of water 2 days before the procedure and the day before. This is to prepare your kidneys to flush out the dye used during the procedure.
You normally come in the same day as the procedure at 7am in the morning. Unless there are plans for you to come in the day before, you should make your way to your allocated ward.
The night before the procedure you should not eat any food from midnight. You can sip water until your procedure. You should take your normal medicines in the morning unless you have been told to withhold them at pre op.
You may have some blood taken before the procedure.
You will normally start anti platelet medication up to 7 days in advance if you are not already taking it. These drugs are most commonly aspirin and clopidogrel although others may be chosen. The purpose of these drugs is to reduce the risk of the blood clotting during the procedure and so it is important you take them.
If you have certain medical conditions, you may need to come in the day before.
If you take anticoagulation medications such as warfarin, this will be reviewed by your specialist nurse at pre-operative clinic and you will be advised when to stop your medication and when to recommence it.
Before any procedure consent must be obtained. A doctor will explain the risks, benefits and how they will do the procedure before they gain your consent. At this time you can ask questions about the proposed procedure. Please do not hesitate to ask any questions.
Every effort is made so that you can have your procedure on the planned day but unfortunately, if another patient comes in as an emergency, your procedure may need to be postponed. Emergencies will always take priority.
Although you are not likely to need one; if there are no intensive care beds your procedure will be cancelled as your safety is our priority.
We will make every effort to prevent cancelling your procedure. If it is cancelled, you will normally go home and return a second day.
What happens during the procedure?
Carotid or vertebral artery stenting is a delicate procedure that may take a couple of hours or longer. During the procedure you will be closely monitored by medical and nursing staff.
Local anaesthetic is injected through the skin and into the groin and a needle is then used to enter the artery. A wire can then be passed through the needle and then a catheter (a plastic tube) is inserted into the artery while under x-ray control.
The catheter is guided up to the carotid artery just below the narrowed area. Part of the catheter has a deflated medical balloon with a stent over it. The balloon and stent are carefully placed across the narrowed section of the carotid or vertebral artery. A balloon is then inflated, this helps to widen the artery and the stent then opens and embeds against the artery wall. There may be a brief discomfort in the neck but this usually goes away.
Once the stent is in place, the balloon is then deflated and removed. This will then leave the stent supporting the arterial wall. The catheter will then be removed and then pressure is applied to the groin area until bleeding has stopped. Sometimes a plug is used to help stop the bleeding.
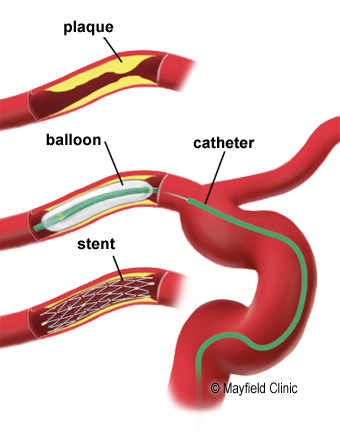
(Picture from google images mayfieldclinic.com)
What happens after the procedure?
Once the procedure has finished, you will then spend time in the post-operative care unit (recovery). You will be closely monitored and then go back to the ward once it is safe to do so. On rare occasions, it is necessary for you to go to the critical care unit where there are more facilities to treat and monitor you, if that is what your interventional radiologists recommends.
What are the risks of stenting?
The procedure will be carried out unless the benefits outweigh any possible risks. You will have discussed the procedure and the risks associated with your neurologist/interventional neuroradiologist/neurosurgeon. You will have given your consent before you go ahead with the procedure.
- Stroke or stoke-like symptoms such as weakness or numbness in an arm or leg, problems with speech
- Bleeding/bruising - almost all patients have some bruising at the groin
- Sometimes damage to the arteries due to the catheter
On return to the ward
Once you return to the ward, you will need to lie down on bed and rest for up to 6 hours which helps to minimise the pressure on the artery that has been used to access for your procedure.
You will have regular observations of your conscious level, blood pressure, heart rate, puncture site and pulses in your feet. You will also have a drip to make sure you don’t get dehydrated. Once the drip has been removed, it is expected that you will drink at least 2 litres of water the next day as this helps to wash out the contrast (dye) used in the procedure.
You will have stockings or compression devices on your legs until you have started mobilising. You will also have blood thinning injections that are given via a small needle into the stomach until you go home. This is to prevent venous clots (DVT) in your legs while you are not moving around as much and will be discontinued when you get home or you are moving around normally.
You will normally be commenced on two antiplatelet medicines which are usually aspirin and clopidogrel after the procedure if you are not already taking them. The type and duration of these medicines depends on the advice your consultant interventional neuro-radiologist as well taking account of stroke doctor gives.
Eventually you will be allowed to sit up and gently mobilise with supervision if the nurse looking after you feels it is safe to do so.
The puncture site in your groin is sometimes painful afterwards. There may also be some bruising and swelling. Occasionally this can be excessive. If you do notice this then you must inform the nurse looking after you or your medical team. The site should not bleed afterwards but it is advisable to hold this area to support it whilst coughing or straining afterwards if possible.
When will I go home?
You will normally have blood samples taken to make sure your kidney function is stable the day after the procedure. Rarely, the contrast (dye) can make your kidney function worse (more so if there is a pre -existing problem).
Once your medical team are happy that you are recovered and your blood tests are satisfactory, you will be allowed to go home. This is often the day after the procedure if there were no complications.
You will go home on a course of anti-platelet medication such as aspirin and/ or clopidogrel. You should have clear instructions on the dose and length of time you should take this before you go home. Please ask your medical team, specialist nurse or ward nurse for the instructions for your medication. You should not normally stop this medication unless you are advised to do so by your medical team.
Aspirin can sometimes worsen ingestion or heart burn and may make breathing worse in those with asthma. Occasionally, it can cause bleeding or skin reactions. If these side effects occur seek medical advice. Clopidogrel can rarely cause stomach upset, excessive bruising and bleeding problems.
In the rare event you get excessive bruising or bleeding please contact you’re G.P and/or contact us for further advice. You may need a blood sample taken to check on your blood clotting if this happens.
Can the stent move?
The tissue cells of the artery wall begin to grow over the stent and the stent will become part of the artery wall.
Follow up
You will usually be reviewed in clinic in 2-3 months by your consultant neurologist. It depends on your consultant neurologist if you require any further follow up imaging.
Some advice for recovery
Whilst there are no scars from this procedure, please be aware that you may need time to recover as it is a delicate procedure. You may feel a little ‘under the weather’ or tired for a week or so following the procedure.
Discomfort of the neck
You may have some discomfort in the region of the stent for a period of days to weeks, but this usually improves by itself.
Headaches
Headaches may occur following the procedure. They usually ease after a few weeks. Simple medications such as paracetamol should help. Headaches can be triggered by dehydration, stress, too much or too little sleep and missing sleep. Drinking 2 litres of water a day should help reduce the frequency and severity.
A rare risk that could occur after stenting is something known as ‘Cranial Reperfusion Injury’. Severe headaches within the first month of the procedure are a sign of this. If you experience severe headaches you must seek urgent medical advice. These headaches develop as a reaction of the brain as blood flow is restored to the brain.
Hair loss
Very rarely small patches of hair loss can occur after any treatment involving x-rays. The hair usually grows back.
If you do lose some hair, you should use gentle shampoo only and not use strong chemicals such as dyes, perms and strong hair products
If this happens to you, you should let us know.
Pacing
Recovery is helped by pacing your activity for the first week or so following going home. Take a daily rest as well as some gentle exercise. Build up activity as you improve.
Returning to work
You can return to work as soon as you feel able although most people need about 2 weeks off to recover. (Occasionally more if there have been complications).
Commonly asked questions
Driving
Driving involves many different cognitive and physical skills as well as multi-tasking, decision making and problem solving.
Driving restrictions following a stroke or TIA symptoms depend on your individual symptoms and should be guided by your stroke doctor or neurologist.
If you have permission to drive you should avoid it for 7 days after the procedure as the arterial puncture site heals
Flying
You should be able to fly as soon as you feel able. It is safe to go through the metal detectors in the airport; they do not affect the stent. You should always inform your insurance company before flying.
Smoking cigarettes
Smoking cigarettes is one of the major risk factors for atherosclerosis/ cardiovascular disease; it is advised that you give up smoking completely. A free help line number is printed at the end of this booklet.
Drinking Alcohol
Whilst alcohol in moderation is acceptable it is advisable you reduce the amount you drink if excessive.
The government suggests that to keep health risks from alcohol low then don’t drink more than 14 units a week and spread over 3-4 days. Information websites on alcohol awareness is printed at the back of this booklet.
Sexual Activity
You can resume normal sexual activity as soon as you feel able.
Sport and swimming
Most sports can be resumed gradually once you have recovered, although it is best to avoid extreme and contact sport until you have seen your consultant neurologist.
Hair washing and hair dyeing
You can wash your hair as soon as you feel up to it. The stent will not be affected by dyeing or perming your hair.
Dental treatment
Dental treatment is safe after the stent has been inserted however your dentist may not be happy to treat you whilst you are taking aspirin and clopidogrel. Your dentist should contact your stroke doctor or GP for further advice if you need treatment whilst taking aspirin and clopidogrel.
Is there anything I should do?
As you had contrast (dye) during your procedure, it is really important that you drink at least 2 litres of water over the next few days. This will help your kidneys work and help flush out the contrast.
What to look out for when I go home?
Seek urgent medical advice if you experience any of the following:
- Bleeding or lump getting bigger in the groin
- Any weakness in your arms or legs, altered sensation, slurred speech or visual problems
- Sudden onset of severe headache or worsening headache
- You become more drowsy
- You should be aware that sometimes a rash can develop. This can be related to the contrast (dye). It is usually mild and does settle however if the rash is severe, please seek medical advice.
If you have any concerns or would like advice after discharged you can contact the ward, your stroke doctor or neurovascular nurse. Contact numbers are at the back of this booklet.
Contact Details
For any emergency see your G.P or your go to your local Accident and Emergency Department
Patient Experience Team provides a PALS service - 0151 556 3090/3091
wcft.patientexperienceteam@nhs.net
Neurovascular Nurse Specialists: 0151 556 3325 Or through hospital switch. (Non-urgent enquiries – calls may not be answered the same day)
Walton Centre switchboard - 0151 525 3611
For information regarding appointments or DVLA contact your Consultant’s secretary.
Useful contact details
NHS 111: 111
Telephone advice if you need urgent medical help fast but it is not a 999 emergency (or you do not have a GP)
Website: http://www.nhs.uk and search ‘emergency and urgent care’
D.V.L.A. Driver Vehicle Licensing Authority,
Drivers Medical Group, DVLA, Swansea, SA99 1DL.
Medical Enquiries: 0300 790 6806
The Brain Charity: 0151 298 2999. www.thebraincharity.org.uk
Working Life Service at The Brain Charity: 0151 298 3288
Department of Work and Pensions: 0345 606 0265
NHS Free smoking helpline: 0300 123 1044
Advice on Alcohol: www.drinkaware.co.uk or www.drinkingandyou.com
- Last Updated:01 June 2023
- Review Date:01 June 2027
- Author:Selina Monahan
- Summary:
Carotid or vertebral artery stenting is an endovascular treatment which means it is performed through a blood vessel by a consultant interventional neuro-radiologist. The procedure is usually carried out under local anaesthetic.