Sacral nerve stimulation
Sacral Nerve Stimulation
Sacral nerve stimulation (SNS) is a treatment option, initially developed for people suffering with bladder control problems (difficulty with bladder function for example not feeling the bladder filling or having very little warning to pass water). It has since been found to be useful in faecal (bowel) incontinence and also constipation. It is also considered on an individual basis in some cases of pelvic pain.
What does the procedure involve?
This procedure initially involves trial by temporarily stimulating the nerves in the sacrum which supply the organs in the pelvis and the pelvic floor muscles using thin electrodes (wires) which create gentle pulses of electricity. The temporary or ‘trial’ period of stimulation over two weeks is to see if the stimulation alters bladder or bowel function or controls the pain. If the test is successful, a permanent lead is placed into the sacrum and a battery implant is inserted into the buttock area.
What are the alternatives to this procedure?
Bladder re-training, physiotherapy, drug treatment, Botox injections into the bladder, posterior tibial nerve stimulation, bladder enlargement or, urinary diversion into a stoma.
The reason for a sacral nerve Stimulation trial
Sacral nerve stimulation (SNS) is not effective for everyone. We therefore do a trial of stimulation which lasts up to two weeks, to see if it will be of benefit to you.
The Trial
The test stimulation involves coming into hospital to have the electrode inserted. This is carried out in the operating theatre under local anaesthetic. You will be given fasting instructions based on your timing of the procedure.
Risks/benefits/alternatives
There is a small risk of infection at the site of insertion of the temporary electrode. For further information regarding possible complications with a permanent implant please refer to the Medtronic patient therapy guide. This will be made available to you if the test period is successful, prior to insertion of permanent implant. The intended benefit of SNS is to improve bladder or bowel function and is an alternative treatment option to failed conservative therapies such as changes to diet, medication and biofeedback.
Battery replacement in external box
Although it is hoped that the battery in the test box will last for the duration of the test, this cannot be guaranteed. When the box is switched on, the flashing green light indicates that the battery is fine but if the colour changes to orange, this indicates that the battery needs to be changed. The battery is easily changed and should be disposed of. The test box uses ordinary 9V battery.
Removal of test electrode
You will be given an appointment to return to hospital about 2 weeks following insertion of the test electrode so it can be removed. Removal of the electrode is very simple and does not require an anaesthetic. It is no more uncomfortable than having stitches removed. Bring your diary with you so that it can be determined if the test was a success. If successful then your consultant will discuss with you the next step in your treatment.
The Permanent Implant
Your hospital stay for this procedure is normally one to three days. To provide more time for preparation, it is usual to come to hospital the day before surgery. The operation takes about two hours and is usually done under local anaesthesia and or deep sedation.
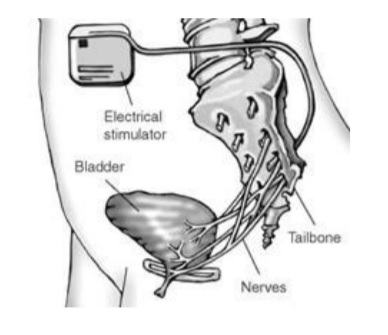
The operation involves placing an electrode around the sacral nerves and is gently secured. The other end of the lead is passed under the skin, and connected to the pulse generator (battery), which is positioned in your buttock area under the skin (see picture). All the parts are completely enclosed inside your body. However, it is common to be able to see and feel the outline of the pulse generator.
In Theatre
You will be assisted to lie on the theatre table, face down. An x-ray machine will be positioned over you so the doctor can accurately see the bones of your lower spine and sacrum. Under aseptic (sterile) conditions local anaesthetic will be injected to numb the skin where the trial wires will be passed through a hollow needle, into the sacrum so that the electrode can lie alongside the sacral nerves. The wire is then adjusted with the help of X-ray monitoring until it is in the right place. A hand-held device that produces a mild current is then connected to the wire. It is switched on and adjusted until you feel a strong tapping sensation in your pelvic floor area and around your rectum and in your big toe. These sensations alongside certain muscle responses confirm to the doctor the correct location of the electrode. On completion, the needle is then taken out leaving the wire in place, and the electrode is covered by a large dressing and connected to the external battery box.
It is vital that this electrode does not move during the test period.
On Return to the Ward
When you return to the ward, the specialist nurse or physiotherapist will visit you to inspect your dressing, ensure you feel okay and answer any of your questions. They will reconnect the hand-held device to your wire and aim to reproduce or improve upon the sensation you felt in theatre. You will be shown how to use the hand-held device and will also be asked to complete bladder volume diaries so any change to your condition in response to the stimulation can be assessed.
Dependent on your wound and response to the stimulation you may be allowed home the same or following day. You will be asked to return to the hospital on certain days to have your dressing inspected and review your on-going response.
During the trial it is extremely important you keep your dressing dry and clean. This unfortunately means you will be unable to have a bath or shower for the duration of the trial and you will be asked to strip wash instead. This is to minimise the risk of infection. Once the trial has ended you will be able to wash as normal.
After the Operation
Later that day or the next day, your stimulator will need to be switched on and fine tuned to give the best possible sensation in the desired area (programmed). The specialist nurse or physiotherapist will do this using a hand-held computer that can communicate with your implant through the skin. As with the trial, you will feel the tingling in the area of your pain. You will also be shown how to use your own hand-held programmer.
It is usual to have significant back/buttock pain during the first few days after surgery. However, you will be given painkillers to help reduce this and it usually settles after a few days. It is important to perform gentle and regular movement to reduce your pain.
Once you are well enough, confident in using your programmer and it has been arranged for your staples/stitches to be removed 7-8 days after your surgery, we will arrange your discharge.
Once you have had the surgery and in the long-term, it is important to avoid activities that could put undue stress on the implanted system because this could cause damage or movement of the system. Do not do activities that include sudden, excessive or repetitive bending, stretching, twisting or bouncing.
Possible complications
Failure or breakage of part of the system, and movement of the electrode from the correct position. These are fairly minor problems that can usually be corrected with further surgery.
Wound infection, damage to the spinal cord, Meningitis and bleeding, or infections around the spinal cord are rare complications but could be life threatening.
To help minimise this risk it is extremely important that you keep your dressing dry and clean as you did during the trial. This unfortunately means you will be unable to have a bath or shower until your staples are removed at 10 days post operatively. Once the staples have been removed you will be able to wash as normal.
Frequently Asked Questions
How long will it take me to get back to normal activities?
Occasional light lifting…………………………… 3 weeks after surgery
Work and driving…………………………………. 4 - 6 weeks after surgery
Heavy lifting……………..………………………... 12 weeks after surgery
These timescales are only a guide and may vary for different people.
How long do the stimulator batteries last?
The stimulator battery can last up to five years with 16 hours use per day. The battery can usually be replaced as a day-case procedure using local anaesthetic.
How will I know my battery is running down?
We will check the battery life regularly during your clinic appointments. However, if the battery is running low you may feel a reduction in the effect and the battery light on your hand-held programmer will flash.
Can I drive with the stimulator on?
No. It is not safe to drive or use potentially dangerous equipment with the stimulator turned on. You may get a surge from your stimulator that could affect your control. If your relief lasts for some time after switching the device off then you may wish to apply stimulation before you drive. You may also want to take regular breaks in your journey to apply a top up.
Can magnetic fields and electrical equipment affect the stimulator?
Yes. It is best to keep away from the following:
- Small magnets (including magnetic strips in freezers and fridges) – keep at least 25cm (10 inches) away from the stimulator.
- Computer disk drives.
- Household power tools – keep at arms length.
- Radios, phones (cordless, mobile and conventional) – keep at least 10 cm (4 inches) away from the stimulator.
- Large industrial equipment – may reset stimulator to factory settings.
- Electric substations – keep at least 8 metres (25 feet) away.
- Arc welders – may cause a shock or a jolt, even when the stimulator is off .
Most household electrical equipment that works properly and is properly grounded will not interfere with your stimulator.
Will security devices interfere with the stimulator?
Certain theft or security devices may cause inappropriate or additional stimulation. Approach these devices slowly and if your stimulator is affected switch it off whilst you pass through the device. The stimulator may cause certain security devices to alarm, for example those found in airports, shops etc. Before you leave the hospital you will be issued an ID card to carry with you in case this occurs.
Will any medical treatments or investigations interfere with the stimulator?
It is important to let your dentist, physiotherapist, doctors know that you have a stimulator before you attend for any treatment or investigations.
The following treatments / investigations may interfere with your stimulator:
- MRI scans (used in X-ray departments)
- Short wave diathermy (used in physiotherapy)
- Electro cautery (used during operations)
- Lithotripsy (used to break up bladder, kidney and gallstones)
- Radiotherapy (used in X-ray departments for cancer treatment)
- Bone growth stimulators (internal or external)
- Ultrasound (used in X-ray department and physiotherapy)
- Cardio version/ defibrillation/ pacemakers (to treat irregular heart rhythms)
The following treatments / investigations should not interfere with your stimulator, if the precautions below are followed:
- TENS machines - the electrodes should be at least 10 cm away from the implanted system (including the leads).
- Mammograms - it is advisable to turn your stimulator off.
- Laser treatment - avoid directing over the implanted system (including the leads).
- Dental drills, mixers and ultrasonic de-scalars that are properly maintained - keep at least 15 cm away from the implanted system (including the leads), but it is advisable to turn your stimulator off.
- Standard x-rays will not interfere with your stimulator.
Can I go on board a plane?
Commercial flights will not affect your stimulator.
When can I return to sport?
Avoid contact sports as they could lead to electrode damage. You can return to activities like swimming when your wounds have healed. You should gradually build back up to other sports over the following six to eight weeks.
This leaflet is only a guide. For clarification and current information, please consult your Medtronic User Manual issued to you with your hand-held programmer.
Or a non-urgent malfunction of your system
What happens if I have any problems?
If you have a query regarding a clinic appointment, or a non-urgent malfunction of your system, please call:
Neuromodulation Service Secretary on 0151 529 5675
If you suspect you may have an infection or you have an urgent query and it is between 9.30am and 4.30pm Monday to Friday, please call:
Nurse specialists: On 0151 529 5647
Or
Specialist Physiotherapists: On 0151 529 5965
If you suspect you have an infection or you have an urgent query and it is after 4.30pm or it is a weekend or bank holiday, please call
Switch board on 0151 525 3611 and ask them to contact the senior nurse bleep holder at the Walton Centre.
- Last Updated:01 September 2022
- Review Date:01 September 2024
- Author:Neuromodulation Team
- Summary:
Sacral nerve stimulation (SNS) is a treatment option, initially developed for people suffering with bladder control problems (difficulty with bladder function for example not feeling the bladder filling or having very little warning to pass water).