Cauda Equina Syndrome
Introduction
Cauda Equina Syndrome is a complex condition that can cause difficulty with nerve messages being sent from the brain down the spinal cord to the lower spinal nerves and back to the brain from the lower body. The following information is designed to help you understand what cauda equina syndrome is and how it could affect you. Please remember every patient is different and there are different degrees of recovery for each individual.
Normal Spine Function
To explain the condition it helps if we begin by explaining the normal spinal function.
The Spinal Column consists of a set of bones that all sit on top of each other to form a tower of bones that protect the delicate spinal cord and the nerves that run through a channel in the centre of this tower of bone.
In between these bones sit inter-vertebral discs, these are soft cushions of tissue that act like shock absorbers for the spine. They protect the bones from rubbing on each other as we move and allow us some flexibility in the spine.
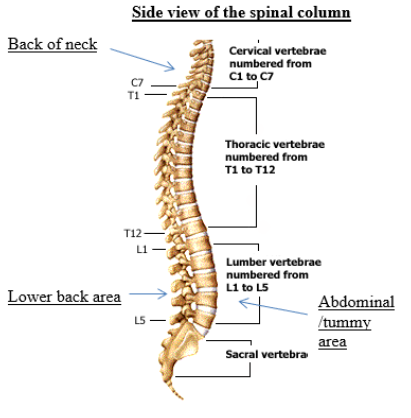
At the level of each vertebra a pair of nerves leaves the spinal cord, travelling through specific holes in the bony column (foramina), one nerve on the right side of the spinal column and one on the left. These nerves pass messages from the brain to the body and back again, acting like a telephone exchange or internet highway.
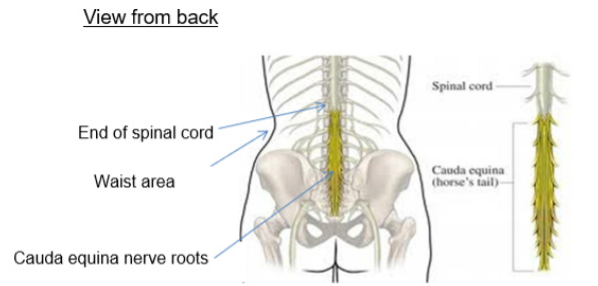
In the lower part of the spine, the spinal cord finishes at about the level of lumbar vertebra 1 or 2, and beyond this it becomes a big bundle of nerve fibres, known as the cauda equina nerve roots. This bundle of nerves are responsible for the messages of movement and sensation to the legs, feet and saddle (bottom and genital) area. They also have a significant involvement with bladder, bowel and sexual function.
What Causes Cauda Equina Syndrome?
Cauda Equina Syndrome occurs when the cauda equina nerves are put under pressure or squashed. This can be caused by many different reasons for example -a large disc prolapse (slipped disc), a tumour or spinal fracture. Although the cause of this may be very important to you, it is the consequences of the pressure to the nerves that cause your symptoms and need to be managed correctly.
The big bundle of nerve fibres in the lower back become squashed and this creates difficulty for any messages to be passed through them, as a result this causes problems with function.

MRI Scan, view from the side, showing a prolapsed disc compressing the cauda equina roots.
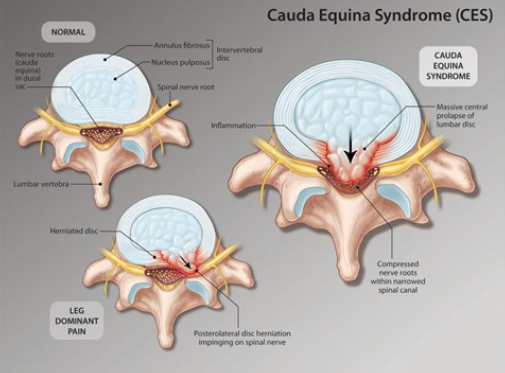
This diagram is looking at the spine from the top downwards.
You can see on the far-right picture how the prolapsed disc is filling the spinal canal where the cauda equina roots are positioned and compressing them.
As the nerves in the bottom of the back control feelings and movement in the lower part of the body, it is the legs, feet, bladder, bowel and sexual functions that can be affected.
For some patients the first sign that something is wrong, can be pain in the leg or legs, difficulty passing urine, opening the bowels or with weakness in the feet or legs. Parts of your leg, foot or the sacral and genital area (bottom area) may feel numb or strange.
What happens at The Walton Centre?
In most cases you will be referred to the medical staff at the Walton Centre as an emergency, that means rather than attending an out-patient clinic, you will be transferred over to us from your local hospital, as soon as possible, this is often by ambulance and can be at any time of the day or night.
If it is considered necessary then you will be taken for an operation to remove the cause of the pressure on the lower spinal nerves. In most cases this will be a microdiscectomy for a slipped (prolapsed) disc. (There is a separate booklet explaining about the surgery we perform please just ask the ward staff)
The aim of the surgery will be to give you the best chance of improving your symptoms. Surgery cannot repair any damage to the underlying nerves. This means that the underlying nerves need to go through a process of recovery after surgery. In general we would expect you to have made your full recovery at approximately 12—18 months after your surgery. This does not mean that you cannot make progress over a much shorter period of time, but what we cannot do is predict your outcome/recovery as, we do not know how much recovery your nerves will make. We have to wait and be guided by the changes in your symptoms as the recovery occurs.
This can make the recovery process for you very frustrating. There is little we can do to change this, there are no scans that can show us the degree of damage to nerves and/or how severe this is, but we are there to support and advise you through this process.
What affect will Cauda Equina Syndrome have on me?
The honest answer to this question is that we do not know, it varies from one individual to the next and also changes as your nerves recover and improve.
You may experience some of the following problems: -
Difficulty passing urine
Problems with bowel function
Leg pain
Problems with movement or sensation in your legs and/or feet
Altered sensation in your bottom and genital area, such as numbness.
Difficulty with sexual function
Management of this condition varies depending upon how the damage to the nerves affects you. The damage to the nerves may be temporary or permanent, it may be partial, or it may be complete, which means you may have some problems with functions like leg movement for example but not a complete inability to move them, as some messages still work. An individual plan of care will be developed for you, and this is likely to be done with you by the spinal nurse specialist.
The Spinal Nurse Specialist service is there to help you through this and to support you, changing and developing your care plan as your nerve function hopefully improves.
(See contact details toward end of leaflet)
Bladder function
For many patients this can be the first problem that needs to be addressed, and usually needs monitoring whilst you are in hospital.
We will monitor how well you are passing urine from your admission, some patients are admitted to The Walton Centre with a catheter (tube in your bladder often attached to a drainage bag) which has already been inserted in their local hospital. We will remove your catheter and we will record any urine you manage to pass yourself and check that you have emptied your bladder fully. We check how much is left in your bladder by using bladder scanners which are ultrasound machines, and by running a small probe over you tummy they can tell us the volume of urine you have left in your bladder after you have been the toilet.
It is not unusual for you to feel as though you have emptied your bladder, and for us to find it is actually not empty. This is because the nerves that pass messages to tell you how full your bladder is are not working properly.
Retaining urine in the bladder after passing urine can be caused by many things: -
Pain
Affects of anaesthetic medication
Prostate problems (in men)
Affects of some medications
Constipation
Nerve damage
As you can see nerve damage can sometimes be exacerbated by some of the other factors mentioned above, with regard to emptying the bladder.
Your spinal nurse will develop a plan of care for you in relation to managing your bladder, and please remember due to nerve recovery what your bladder function is like on day one, does not mean this is how it will stay, it can often change as nerves recover.
Please see the information book on bladder function.
Bowel function
This is usually the second area of concern. Many patients find they have difficulty passing bowel movements, due to the reduced sensation and the poor ability to push to empty the rectum secondary to the nerve damage.
Without any nerve damage bowel function varies with each individual, so when nerve damage occurs, it can often take time to establish a bowel regime that works for the individual. This usually involves the use of oral medication and rectal suppositories (medication that you place in your bottom)
Your spinal nurse will work through a regime with you and this often requires trialling different medications etc. till we find what works well for you. (Please see the booklet on bowel management)
Pain
Some patients find they still experience neuropathic pain (pain from the nerves that are irritated/damaged) in their buttocks/legs/feet, this often requires use of specific medications to help manage this. Once you have recovered from the surgery, as your pain improves these medications can be reduced.
The most common types of medication for nerve pain are anticonvulsant medications (medications to stop fits) and anti-depressant medications (medications used to treat depression).
This is because these medications are designed to work on nerves, so they are also used for nerve pain. They take time to build up a level to give you maximum benefit so they should be gradually increased, and when you want to stop or reduce them this should be done gradually by weaning off them with advice from your GP or specialist.
Other medications include opioid medications such as Morphine, again once you recover from your surgery these can be reduced.
Standard pain medications can often help with post operative wound pain such as paracetamol or Ibruprofen, and these are easily purchased at most shops.
Some pain after surgery is expected from your wound, and the affects of the operation, some patients find this is easier for the first few days to a week and then once the initial medications from your anaesthetic and hospital stay wear off, and nerve irritation from surgery occurs, there can be a flare up of pain after this. This should settle with time, continue with your medication regularly until you feel comfortable and then you can start to reduce this under the supervision of your GP.
Movement
We will get you out of bed the day after your surgery and the physiotherapist will sometimes see you. It is normal practice to be mobilised the day after surgery. Mobility relaxes the muscles, reduces muscle spasm and helps reduce pain.
If you have any foot or leg weakness the physio will work on this with you, if you need physio after discharge they will arrange this. Any recovery of weakness often takes many months, and in some cases it may not fully recover. It is not possible to predict how much recovery it will make as we cannot see the degree of nerve damage. As nerves recover hopefully your weakness will improve.
You need to work with the physio doing the exercises they give you, even after discharge and attending any physio sessions that are arranged for you.
Sensation
Any numbness you may be experiencing in your legs, bottom area, genitals or between your legs, may improve with time. This often takes some time if it is going to improve, often over many months. There is nothing you can do to change this recovery process, your body and nerves just need time to repair and recover. In some instances this may not recover, or may make a degree of recovery but never return to normal.
Sexual function
Cauda equina syndrome can affect sexual function, in men this can be reduced sensation around genital area and lack of ability or reduced ability to gain an erection or ejaculate, and in women it can be the lack of vaginal and perineal sensation, meaning a reduced ability to feel during sexual activity.
Once again time will produce any recovery that will occur, but again this can take a long time, many months if it is going to occur. There are methods to help men gain erectile function with medications and/or devices, but there is nothing that we can use to improve sensation.
It is often the body’s clever ability to adapt that means other areas of the body will become sensitive and responsive to stimulation. It requires some time and experimentation to learn which parts of the body are now important to you for sexual pleasure. Please speak to your spinal nurse about any concerns or questions you have.
Psychological recovery
The surgery for cauda equina syndrome is often performed as an emergency, in order to give you the best chance of recovery, however, this can cause its own problems as patients often feel quite traumatised by the speed of the process. It gives little time for thinking about what is happening and it is often after surgery that the situation can become quite overwhelming. It is not unusual to feel traumatised, stressed and/or emotional by what has and is happening, so please don’t worry about feeling like this or getting upset. Ask the spinal nurses for any explanations you need and any information you want repeating. If it helps then we can speak to you with a member of your family and explain all that has happened to you so you have additional support. We obviously cannot speak to anyone about you without your permission but if you want us to speak to a family member then please just ask.
It is really important that you do not worry about talking to us about how you feel, about bladder, bowel or sexual dysfunction issues or any concerns, the spinal nurses have spent time with other patients who have experienced the same process and fully understand the situation, so please do not feel embarrassed or worry about difficult conversations.
We will arrange to see you in the out-patient clinic at a time that is appropriate for you and your clinical condition; this can be within a few weeks after discharge or at a longer interval depending on what your individual requirements are.
Should you have any queries or concerns then please feel free to contact us and leave a message on the Spinal nurse contact number Tel: 0151 556 3424 and we will get back to you as soon as possible.
- Last Updated:01 June 2023
- Review Date:01 June 2025
- Author:Keren Smallwood
- Summary:
Cauda Equina Syndrome is a complex condition that can cause difficulty with nerve messages being sent from the brain down the spinal cord to the lower spinal nerves and back to the brain from the lower body. The following information is designed to help you understand what cauda equina syndrome is and how it could affect you. Please remember every patient is different and there are different degrees of recovery for each individual.