Cranioplasty
What is a cranioplasty?
Cranioplasty is the surgical repair of a bone defect in the skull resulting from a previous operation or injury. There are different kinds of cranioplasties, but most involve lifting the scalp and restoring the contour of the skull with a graft made from material that is reconstructed from CT scans of your own skull and so individual to each person such as:
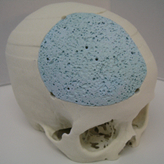
- Solid biomaterial (prefabricated customised implant to match the exact contour and shape of the skull).

- Titanium plate/mesh
Reasons for a Cranioplasty and how they are made?
The goal of the surgery is generally for cosmetic purposes to restore the natural contour and shape of the skull, in addition to providing a rigid protective structure around the brain. In essence, the cranioplasty is performed to replace the rigid bony structure that is missing in the skull.
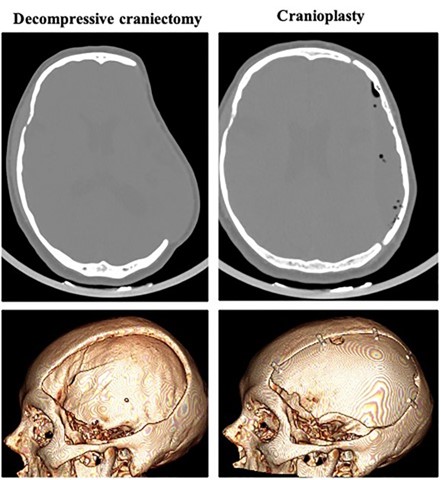
The cranioplasty is prepared prior to the surgery. These are known as “prefabricated” implants. These implants can be designed, and 3D printed to provide excellent results. Once completed, they are sterilised and used during the operation.
Preparing for the operation
You will be seen in the pre-operative clinic where you will be assessed for fitness for a general anaesthetic, explain the procedure and answer any concerns. The pre-operative clinic review takes approximately 1½ - 2 hours in total. Bloods and measurements of height and weight will also be taken. Please bring a copy of any medicines you are taking and a list of your other illnesses and medical conditions.
Further tests may be necessary according to your general well-being and other medical conditions before a decision is made that you are fit for the anaesthetic procedure.
You will be assessed by an anaesthetist before the operation. The anaesthetist is the consultant doctor who administers the general anaesthetic and pain relief during the operation.
You should shower and wash your hair in the solution given to you in preop, as advised, before the operation to clean and reduce the risk of infection. You will normally come in the same day as your surgery unless otherwise stated. You will be expected to make your way to the hospital for 07:30 and present to Jefferson Ward unless specified. You should not eat anything from midnight before coming to hospital. You can sip water until you come in.
Blood thinning medication will be advised to stop for a period of time prior to your operation. Your pre op nurse will advise against any other medications you need to stop prior to you coming in.
What to expect during the procedure
A cranioplasty is performed in a hospital setting whilst you are under general anaesthetic.
A portion of the scalp will be shaved, and a topical cleanser is applied to prevent infection.
An incision is then made in the skin to access the skull bones. The area under the skin is prepared and the plate is attached using small screws
Cranioplasty Risks
All surgical procedures carry some form of risk. Your neurosurgeon will discuss the risks of the surgery prior to you agreeing and consenting for it. The most common risks associated with a cranioplasty include infection, blood clot formation, seizures and stroke.
- There is a risk of infection with all surgical procedures. If this occurs, you may need antibiotics either through a drip (Intravenous) or by mouth. In some cases, the plate may need to be removed. Precautions are typically taken during and after surgery to prevent the development of an infection. You are encouraged to keep the site clean; do not touch it and wash the hair/scalp as instructed afterwards.
- Stopping smoking will also help the healing process as smoking is known to reduce blood flow and slow healing.
- Bleeding. Although rare, there is a risk of bleeding at or around the site of cranioplasty.
- Stroke. Depending on the indication for surgery, there is a risk of bleeding or clots in the brain that may cause stroke.
- CSF Leak. Although uncommon, you may develop leakage of brain fluid at or around the site of surgery. These can be managed conservatively, resolve on their own, or require subsequent surgeries or drains.
- Anaesthesia. Any procedure performed under anaesthesia carries risks of reaction to the anaesthetic administered and may not be related to the cranioplasty reconstruction.
- Numbness. It is not uncommon to develop numbness at the incision sites. This typically improves over 6 months, but in some circumstances may be permanent.
- Facial Nerve Paralysis. Although rare, cranioplasties carry the risk of weakness in facial movement after surgery. This is usually temporary, but in rare circumstances may be permanent.
After the procedure
Once the operation is over you will go to the post-operative recovery unit to wake up and recover from the anaesthetic. You will be looked after there by skilled recovery nurses. Once you have woken up and been assessed by the anaesthetist, you will be moved to the ward. Which ward you go to depends on how quickly you wake up, how long or complicated the procedure was and other medical conditions you may have.
When you wake up, you will have a drip in your hand or arm to give you fluids through a vein. You will have a bandage on your head and you may rarely have a drain under the skin in the head. You are likely to have a catheter in your bladder which will be removed as soon as possible. You may have compression devices or stockings on your legs to prevent complications such as deep venous thrombosis (DVT). DVT is a blood clot in the leg that is at risk of occurring when you can’t move around as much as normal.
Observations will be done of your blood pressure, pulse, respirations, and you will have your consciousness level and pain assessed. Once you are stable you will move back to a ward to recover before going home.
Recovery from Cranioplasty
Recovery can sometimes take longer if there have been complications as a result of the operation or afterwards. There is a very small risk of complications listed above that may lead to a second operation.
Your surgeon is likely to let you home once you are up and about, stable and pain is well controlled. Some people may benefit from input from the therapy team prior to going home. You will be assessed whilst in hospital to see if you would benefit from this further input.
You may experience headaches in the days following the surgery, but these respond well to pain killers that will be prescribed by your doctor. Fatigue is also a common side effect that should subside within the first few weeks.
Some activities may be limited for a period of time after your cranioplasty, and we will provide you with information on any restrictions that you will be expected to adhere to and for how long on discharge.
As the wound heals the stitches can feel tight; this settles after the stitches are removed. The pain from the operation may persist for a few weeks, although will be less severe and the frequency of headaches should reduce with time.
In the early stages, the area around the wound feels numb. This is because the nerves have been cut. As the nerves grow back there is abnormal sensation such as pins and needles which settles over several months. The wound may itch as it heals.
Please do not scratch it as you will risk infecting it.
There is a very small risk the wound site may become infected: Your surgeon may advise you to apply antibiotic ointment to the site regularly for a few weeks to minimise this risk.
Infection is rare because you will have cleaned your hair/head as advised prior to your operation.
Infection can happen later, sometimes after you have gone home. If the wound become sore, inflamed, red, oozes or you get a temperature then you should get in touch with your specialist nurse, GP, consultant or ward for a wound check and assessment urgently.
Some infections require a second hospital stay if the antibiotics need to be given through a vein.
Wound care
You will either have stitches or clips on your scalp that look like staples. These will need to stay in for approximately seven-fourteen days and you will be asked to return to the walton centre for a wound check and for removal of your clips/stitches.
Pacing
You will benefit from pacing activities for the first few weeks following going home. This includes keeping a routine such as going to bed and getting up at the same time each day, keeping hydrated, a good diet and not missing meals. This will help so you don’t get over tired which may slow your recovery. Enlist the help and support of your family and friends to help with household chores if you can. Take some gentle exercise to help build up your stamina each day, for example a short walk building up as you get stronger. You will benefit from an afternoon rest for the first couple of weeks after going home.
Working
Full recovery can take a few months which means you may have to allocate some time off work. The time off work depends on the type of job you do and the level of responsibility or whether it is a very physical role. Most people need about 2-3 months. If you must go back sooner for financial or other reasons; this won’t do you any harm but may mean you take a little longer to recover as you may feel more tired.
Driving
The DVLA requires you to inform them and cannot drive a car until you are completely recovered and haven’t suffered any complications such as infection, seizures, visual or cognitive problems or stroke: This is because driving involves many different cognitive and physical skills as well as multi-tasking, decision making and problem solving.
Hair Care
You can wash your hair using a mild shampoo after 72 hours. You can dye your hair once the wounds have completely healed which usually takes a couple of months
Sex
You can have sex as soon as you feel able.
Seizures
There is a small risk of seizures after any type of brain surgery. The position of certain aneurysms carries a bigger risk of seizure. A single seizure provoked by the operation does not mean you have epilepsy.
If you do have seizures, you will be given information on safety for your protection. Alternatively, you can log on to epilepsyaction.org
Flying
It is advisable not to fly for 6 weeks after your operation, if you live in the Isle of Man and have flown for your treatment, you will have to take the boat or sea cat home.
Exercise
You can build up your exercise regime gradually as you feel able once you have recovered from the operation. Do not do any extreme exercise or contact sport for the first six months to allow the bone and wounds to heal. If you want to become involved in extreme or contact sport, you should speak to your neurosurgeon or neurovascular nurse for further advice as you would need to have each type assessed individually and understand the risks. Safety helmets should also be worn as with any bone that has been opened or broken it will never be a strong as before.
Alcohol
It is advisable not to drink alcohol until you feel recovered as you will be more susceptible to the effects. You are at a small risk of a seizure the first year after brain surgery and alcohol is known to lower seizure threshold making you more vulnerable to a seizure.
Smoking
Smoking is not recommended as impairs wound healing. Smoking cessation clinics are linked to every G.P. practice or you can ask for help during your stay in hospital. An advice number is printed at the end of this leaflet.
Walton Centre Contact Details
For any emergency see your G.P or your go to your local
Accident and Emergency Department
For information regarding appointments or DVLA contact your consultant’s secretary
Patient Experience Team provides a PALS service.
0151 556 3090
Neurovascular Nurse Specialists: (practical advice; answerphone)
0151 556 3325.
Walton Centre switchboard - 0151 525 3611
Dott Ward -0151 556 4276 / 3887
Cairns Ward - 0151 556 3886 / 3587
Caton Ward -0151 556 3894 / 3588
Caton Short Stay Ward – 0151 556 3567 / 3568
Chavasse Ward - 0151 556 3897 / 8262 / 3591
Lipton Ward – 0151 556 3383 / 3901
Intensive Care - 0151 556 3462 / 3789
Jefferson Ward – 0151 556 3871
Useful Contact details
NHS 111: 111
Telephone advice if you need urgent medical help fast but it is not a 999 emergency (or you do not have a GP)
Website: http://www.nhs.uk and search ‘emergency and urgent care’
D.V.L.A. Driver Vehicle Licensing Authority
Drivers Medical Group, DVLA, Swansea, SA99 1DL.
Medical Enquiries: 0300 790 6806
You can now email the DVLA via www.dvla.gov.uk
The Brain Charity: 0151 298 2999.
www.thebraincharity.org.uk
Offers practical help, emotional support and social activities for people with neurological injury. And their families/carers
Stroke association: 0303 3033 100 www.stroke.org.uk
Offers practical help, advise and local support groups
Headway: 0808 800 2244 www.headway.org.uk
Offers support to improve life following brain injury
Epilepsy Action: 0808 800 5050 www.epilepsyaction.org.uk
Offers practical help for people who have seizures
NHS Free smoking helpline: 0800 0224 332
www.nhs.uk/smokefree
England: 0300 123 1044 Wales: 0800 085 2219
Advice on Alcohol: www.drinkaware.co.uk or www.drinkingandyou.com
- Last Updated:27 January 2023
- Review Date:27 January 2025
- Author:Beth Rooney
- Summary:
Cranioplasty is the surgical repair of a bone defect in the skull resulting from a previous operation or injury.