Discharge guide for patients with a brain tumour
A discharge guide for patients with a brain tumour
Introduction
This booklet provides information and answers to questions often posed by patients following brain tumour surgery. Going home can feel a bit overwhelming. You will have a lot of information to process and we are aware that you or your family may have additional questions, or may want more detailed answers. If this is the case you can contact the Clinical Nurse Specialist (CNS) Team on : 0151 556 3778 or 0151 556 3449 if you are a skull base tumour patient.
Going home — The next steps
Often, when you are going home the results of your biopsy confirming the tumour type will not be available, but once received you will be contacted by your Consultant’s secretary to come to clinic to discuss the results, and what the next steps will be. They will contact you via telephone.
This can be a difficult time as you are in limbo without having any kind of plan. If you need to talk about this the nurse specialist team and the support worker are here to help and support you.
Common symptoms post-surgery
Some patients recover very quickly following surgery, and others take longer. No two people will feel the same.
Some of the most common symptoms are listed below:
• Tenderness & numbness around the wound area
• Mild headaches that should resolve with regular taking of simple pain relief like paracetamol
• Swelling/Bruising that should resolve in the days/weeks ahead. This can also be seen around the eyes and face which can appear alarming but is not cause for concern.
• Tiredness and fatigue
This is probably the most common following surgery and regaining good energy levels can take up to 6-8 weeks. Some tips to help with this are
- Allow yourself time to recover and don’t expect too much too soon.
- Try and build up stamina and exercise tolerance slowly, a gentle walk is a good place to start. Exercise is good for you and will help with overall recovery.
- Allow time to rest, if you feel tired listen to your body and avoid over exertion.
- Eat a balanced diet
• Poor balance can sometimes be experienced after surgery but this should also settle over time and possibly with intervention from additional therapy in the community.
• Noises or whooshing sensations - During recovery you may notice some unusual sensations in your head as things are settling down. These are often described as “crackles, pops, whooshes or drips”. If you have had surgery near your ear, you my experience a dull earache.
All of these symptoms will settle over time
The following brain charities are useful for support and advice following your surgery.
- The Brain Tumour Charity 0808 800 0004 www.thebraintumourcharity.org
- The Brains Trust 01983 292 405 brainstrust.org.uk
- The Brain Charity 0151 298 2999 thebraincharity.org.uk
- Macmillan 0808 808 0000 macmillan.org.uk
All of these charities can provide a wealth of support information, knowledge and advice across a range of things including emotions, finances, benefits, counselling, employment support as well as resources to help you following your diagnosis that can help you talk to family members and children with. Macmillan also have support centres in some of the larger hospitals locally where you can attend and obtain advice and support.
Coping Better Together Course
This is a course for patients and families affected by brain tumours and is run by a CNS from the Walton Centre. It provides useful information and an opportunity to speak to other people with similar experiences. You will be contacted by post with an information pack about this when the course is next available. This is now also run as a virtual event for those who are unable to attend in person or who live too far away from the Centre.
Patient Experience Team
The Walton Centre Foundation Trust, Lower Lane, Liverpool, L9 7LJ 0151 556 3090
The teenage and young adult (TYA) cancer service, The Clatterbridge Cancer Centre.
The team at Clatterbridge support patients aged 16-24 who have a cancer diagnosis. Support includes coping mechanisms, financial issues, educational/ employment needs and social opportunities. Telephone 0151 556 5122 (main office) or 0151 252 5199 (Alder Hey)
Your GP and Practice Nurses, community district nurses - these can all be contacted via your GP Practice.
Local Brain Tumour Support Groups
Liverpool Brain Tumour Support Group - This support group is run by people whose lives have been affected by a brain tumour diagnosis and is available to both patients and those close to them. The group meets on the last Monday of the month 1-3pm at The Brain Charity, Norton Street Liverpool. Contact Steve Sharman on 01606 45357
Northwich Support Group - Everyone is welcome at the Northwich support group which is held at Northwich Carers, this takes place on the first Monday of the month from 1-3pm at Northwich Carers Centre, London Road Cheshire CW9 5HH. Contact Steve Sharman on 01606 45357.
Red flag symptoms
These are the things we want you to watch out for when you get home , as they may need urgent medical attention.
• Your wound becoming red or sore or leaking any kind of fluid or pus. If it is leaking clear fluid or pus we will need to attend the Walton Centre or your local A&E so that we can assess it more thoroughly.
• A soft fluid like swelling behind or close to the scar may develop. This is a collection of brain fluid accumulating under the skin and is called a pseudo meningocele. This usually settles down on its own but please contact us for advice. We may ask you to send us a photograph for us to assess it.
• Nausea or vomiting
• Worsening or severe headache
• Increase in number or change in seizures
• Increased drowsiness, or confusion
If you experience any of these symptoms you should contact us straight away via the emergency bleep on : 0151 525 3611 and ask for bleep 5391. If you are a skull base patient contact their CNS Team on 0151 556 3449 or 0151 529 3611 and bleep 5342 Outside of office hours you should contact Cairns Ward on 0151 529 5638 or 5637, or the ward you were on.
Things to avoid
Driving — see further information below. Any activities that cause you to hold your breath or push, like lifting
FREQUENTLY ASKED QUESTIONS
When will the stitches/sutures/clips be taken out?
This usually happens 7-10 days after surgery. If you are fit and well you will most likely be asked to attend your local treatment rooms or GP practice depending on your local area. Sometimes we will ask for the District Nurses to attend to you at home , but this is normally only if you have mobility or other health issues. The ward will clarify the arrangements and dates with you before you are discharged.
Do I need to continue taking my steroids after I go home?
Yes, it is important that you keep taking the prescribed dose of Dexamethasone, and you will be given specific instructions to either: Reduce the dose over a set time until you are no longer taking any steroids or Reduce to a specified dose until your clinic appointment. Ensure you continue to take your stomach protection tablets whilst taking steroids. If you are running low on either of these a repeat prescription can be obtained from your GP. You can take a copy of your TTO Prescription slip that is given to you with your medications on discharge to the practice so that they are aware of the medicines you are taking.
Do I need to keep taking my anti-seizure medication after my operation?
YES. It is very important that you continue to take this even if you haven’t experienced any further seizures. Some patients require long term anti-seizure medication, others for just a few months following surgery. This should only be stopped on advice from the medical team and should be continued unless advised differently from your consultant.
Useful contacts
Appointments:
For follow up with your consultant please ring the secretary
Mr Brodbelt/Chavredakis 0151 556 3345
Mr Lawson/Jenkinson 0151 556 3346
Mr Zakaria 0151 556 3336
Mr Olubajo 0151 556 3337
Mr Farah 0151 556 3351
Miss Gilkes 0151 556 3347
Mr Yousaf 0151 556 3350
For scan appointments call Radiology on 0151 556 3681
Who can I turn to for help and support?
Clinical Nurse Specialist Teams at The Walton Centre
Neuro-Oncology 0151 556 3778 or bleep via switch 0151 529 3611 bleep 5391
Wcft.neurooncologynurses@nhs.net
Skull Base 0151 556 3449 or bleep via switch 0151 529 3611 bleep 5342
Wcft.skullbasenurses@nhs.net
Clinical Nurse Specialist Team at Clatterbridge Cancer Centre
0151 556 5850 and ask for Jill Sokratous or Jan Holding
Clinical Nurse Specialist Team at North Wales Treatment Centre 01745 445 259 and ask for Pauline Burford. and can be done at any point after surgery.
These can also be good to help talk about how you are feeling and any symptoms you may be having following surgery.
Clinical Trials
You can ask a member of your clinical team about current research and clinical trials.
Alternative approaches to management
Patients often ask about alternative or additional treatments to help in their recovery. As healthcare professionals we are unable to promote any treatment that is not fully supported by medical evidence but we understand that you may want to look at all of these options. We are commonly asked about:
The Ketogenic Diet - this is a diet that encourages low carbs and increased fats and is being trialled by some specialist centres, currently the Walton Centre does not have an open trial relating to this. More information can be found at “Matthews Friends” (matthewsfriends.org) a charity that specialises in ketogenic dietary therapies.
Cannabis Oil -The use of cannabis oil is highly publicised and many patients want to know more about this option. At this time however we do not have any supporting evidence for this treatment and cannabis based products have not been licensed for medical use for people with a brain tumour.
While I was in hospital my blood sugars were checked every day, do I need this checking at home?
Yes, if you are still taking Dexamethasone at home the ward will arrange for your local district nurses or practice nurse to monitor your blood sugars at home. They don’t necessarily have to be checked every day , and frequency will depends on what they were like during your admission. Your GP Practice or District Nurse team may even give you the equipment to do this yourself at home.
When can I wash my hair following surgery?
You need to wait a minimum of 48hours, but once this has passed you can wash your hair and we would recommend you continue to use Hibiscrub which was given at pre-op until stitches/sutures are removed. Be careful not to rub around the wound area, if water runs on the wound this is fine, and can be just patted dry with a clean towel. If there has been leakage from the wound or a previous surgery you may be advised to wait a little longer. In some cases if dissolvable sutures/stitches are used you may be advised not to wash your hair for 5-7 days.
When can I dye my hair again?
You should wait at least six weeks to allow the wound to fully heal, however if you are going to be having oncological treatment you should double check and discuss with your oncologist.
How long before I can fly?
General guidance from The Walton Centre is that we advise to wait around 6 weeks , this is due to altitude and change in cabin pressure within the aircraft as this may cause noticeable headaches and most patients would prefer to avoid this. If you are having Oncological treatment following surgery it is again best to discuss with your team as they may not want your treatment to be delayed whilst you go away.
When can I drive again?
This depends on a range of factors including: What type of tumour it is, the type of operation and any symptoms experienced. Whilst it is difficult to adjust it is very important that you do not drive.
Driving restrictions are stipulated by the DVLA , and you should notify them once you receive histology about the type of tumour you have , they can then advise you of how long you will not be able to drive for. You can find information about driving after the surgery in the leaflet “Driving and Brain Tumours” which was in your original information pack.
DVLA Telephone number 0300 790 6801 Mon-Fri 8am-7pm Sat 8-2pm www.DVLA.gov.uk. If you live on the Isle of Man then you must notify the Department of Infrastructure to make them aware of your situation
When can I return to work?
This depends on lots of factors, including what you do for a living, the type of tumour you have and any future treatment you may need. Most people need a minimum of 6-12 weeks, although this can be longer if your job requires you to drive, work at height, with machinery or you require further treatment. You can discuss this with the medical team or the CNS for further advice and support. If you are worried about financial issues there are lots of information points that you can access including benefits advice from The Brain Tumour Charity, The Brains Trust or Macmillan. See also the Benefits and Financial Advice for brain and spinal tumour patients in your information pack.
Will I have further scans after surgery?
Yes, the frequency of these will depend on the type of tumour you have and will be individual to you. Initially scans may be more frequently but over time the interval between scans will become longer. The frequency will be advised by the medical team.
What we tell your GP
Your GP will be advised of your hospital admission and will receive:
- A treatment summary, this will give details of your surgery, progress to date and follow up plans. It will be sent to your GP when discharged.
- A medications summary, this gives details of any medications that have been started or changed during your hospital stay.
Additional treatment following surgery
In some cases following surgery it will be necessary to have additional treatment in the form of radiotherapy, chemotherapy or a combination of both. Your treatment options will be discussed with you by the Oncologist following histology discussion and referral to the local Cancer treatment centre. At Walton we work with oncologists from The Clatterbridge Cancer Centre and North Wales Cancer Treatment Centre allowing treatment to be given as close to your home as possible.
Long-term support
If you are having lasting symptoms or worries following surgery the CNS team will be happy to discuss in detail either in clinic or over the telephone. We call this a Holistic Needs Assessment or HNA for short. If you feel that you would like a HNA you can contact the team’s clinical navigator/support worker who will happily arrange and facilitate this. These can be good to help your recovery
How was your experience with us?
Please complete the survey either by scanning the QR Code or by using the following link on the internet:
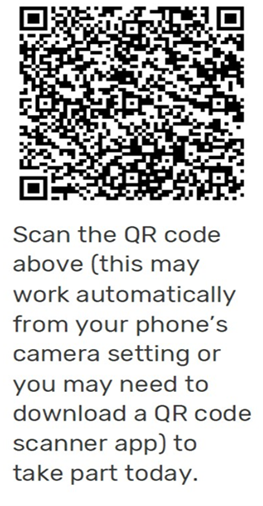
www.thebraintumourcharity.org/care-surveys
It is all anonymous and the data collected from The Brain Tumour Charity is shared with us, to help us improve our care for future patients and their families.
If you would prefer a paper copy of this survey please ask.
- Last Updated:01 September 2022
- Review Date:01 September 2026
- Author:Alison Rodway and Kelly Woods
- Summary:
This leaflet provides information and answers to questions often posed by patients following brain tumour surgery.