Dural Arteriovenous Fistula Of The Brain (DAVF)
WHAT IS A DURAL ARTERIOVENOUS FISTULA?
- It is one or more abnormal connections from an artery supplying the dura of the brain to a vein or venous sinus draining it. The abnormal connection (s) is/are called fistula.
- The dura mater of the brain is the outermost thick membrane surrounding the brain, dural sinuses and the spinal cord. The other two layers are the arachnoid mater (or membrane) and the pia mater. These layers are also known as the meninges.
- As DAVFs grow they may gain more blood vessels and so have a number of fistulous connections making them more complex.

THE VEINS DRAINING THE BRAIN:
- Superficial or cortical veins drain the cortex or outside surface
- Deep veins drain the deep structures in the brain
- These veins ultimately drain into the venous sinuses
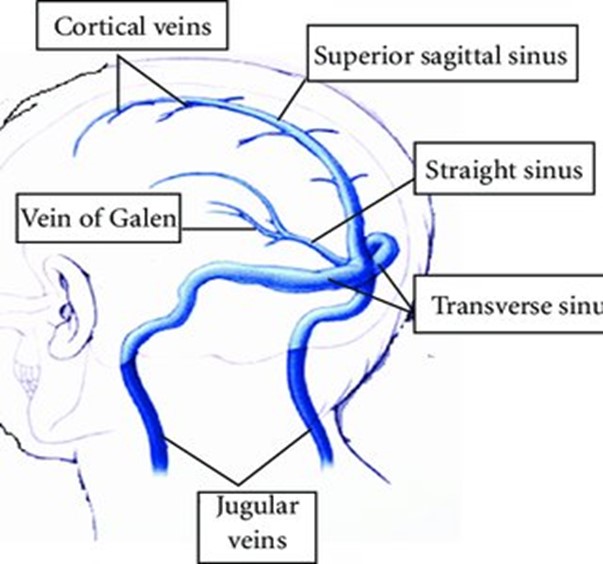
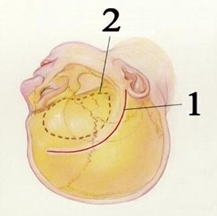
Diagram of the venous drainage of the brain
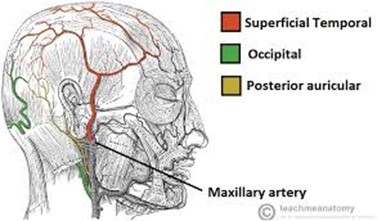
THE ARTERIES SUPPLYING BLOOD TO THE DURA:
ABOUT dural fistulas:
- They account for 10-15% of all arteriovenous malformations of the brain.
- They are different from arteriovenous malformations because they don’t have an origin (or ‘nidus’) in the brain itself
- Most present in adulthood
- There is no single cause for their development
- Most are idiopathic which means they arise spontaneously and so are acquired rather than being born with or hereditary
- Some are thought to develop because there has been a narrowing or blockage to one of the brains venous sinuses causing the body to make new passages (or fistula) to route blood back to the heart.
- Patients with clotting disorders are predisposed to the risk of clots within the sinuses of the brain as well as elsewhere and so this may theoretically make them more susceptible to certain DAVFs
- Rarely patients have a history of trauma or previous brain surgery which is thought may be a responsible cause.
- DAVFs are slightly more common in people with diabetes.
BENIGN Versus AGGRESSIVE DAVFs:
Aggressive DAVFs:
- Aggressive DAVF’s have what is known as cortical venous reflux (this is drainage to the superficial veins of the brain). They are said to be a risk factor for a brain haemorrhage because the veins or fistula can get bigger and bleed.
- The annual haemorrhage rate for aggressive DAVFs is about 8.1% but varies greatly.
- Rarely, some have a higher risk of bleeding and so need urgent treatment.
- Haemorrhage or bleeding on the brain would cause a sudden onset of headache and include vomiting, sensitivity to light and neck stiffness or stroke like symptoms
- Other aggressive symptoms can come about more gradually over days or weeks. These symptoms can occur because of congestion in the veins of the brain connected to the DAVF which in turn causes a reaction in the brain.
- The risk of neurological deficits is about 6.9%
The size and position of the DAVF may mean it can cause compression on important parts of the brain. In addition, the drainage of it may become engorged and cause symptoms including one or more of the following:
- Dementia or reduced cognition (which may or may not improve after treatment) can occur because of congestion in the veins of the brain connected to the DAVF
- Stroke like symptoms or neurological disability
- Speech or language difficulty
- Face pain or headaches
- Noticeable burning or prickling sensation in the head or body
- Seizures or ‘fits’.
- Headaches nausea or vomiting
- Co-ordination problems
- A build-up of fluid within the brain called hydrocephalus.
Benign DAVFs:
These may cause uncomfortable or disabling symptoms such as:
- Pulsatile tinnitus. This is a condition where you can hear the blood rushing through the fistula behind the ear or at the back of head. This sound can resemble a heartbeat and be so loud it is unbearable.
- Headaches
- Visual changes or deterioration in vision
CAVERNOUS SINUS DURAL ARTERIOVENOUS FISTULAS (CSDAVF):
- More benign as there are lots of veins for any arterial connection to drain to and so less likely to build up pressure and bleed.
- Symptoms of CSDAVF include loss or partial loss of vision or movement of the eye, swelling, redness and pain behind the eye due to a build-up of pressure within the eyeball.
- Headache and pain behind the eye.
MANY DURAL FISTULAS ARE COMPLETELY ASYMPTOMATIC OR HAVE MILD SYMPTOMS AND POSE NO PROBLEMS. THESE DON’T USUALLY NEED ANY TREATMENT.
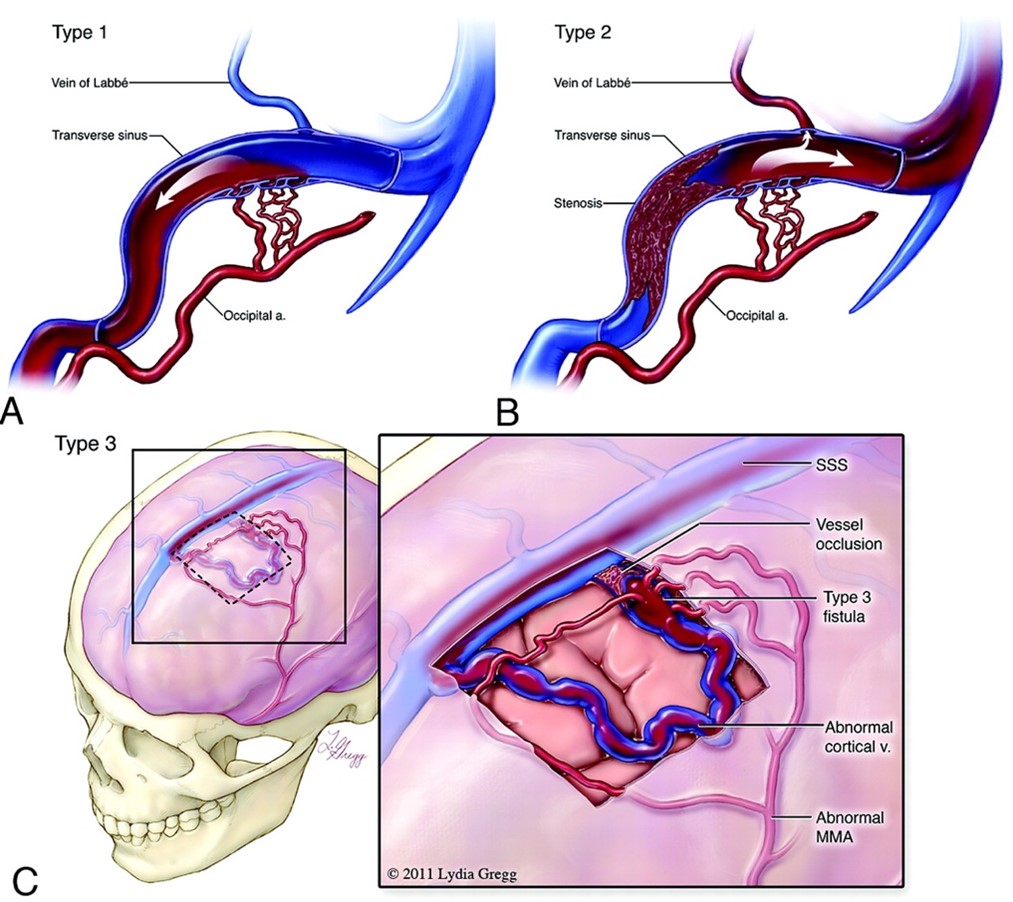
TYPES OF DAVF (Borden system of classification):
Type 1 is classed as ‘benign’. It drains to a venous sinus and doesn’t have cortical drainage. Type 2 is ‘aggressive’. There is drainage to the venous sinus and the cortical veins
Type 3 is ‘aggressive’. There is drainage to the cortical veins.
DIAGNOSIS:
Diagnosis is made through gaining images of the DAVF and its surrounding structures which include
- CT scan of the brain
- CT angiogram of the brain to look at the blood vessels in close detail
- Angiogram of the DAVF
- MR scan of the brain
- Angiogram
What is an Angiogram:
An angiogram is usually undertaken as it allows a management/ treatment plan for the DAVF to be made.
A thin tube is inserted into an artery in the groin. This is passed via the blood vessels to the brain. Dye is then injected, and X-ray pictures are taken. Doctors are able to see the exact location, shape and size of the DAVF.
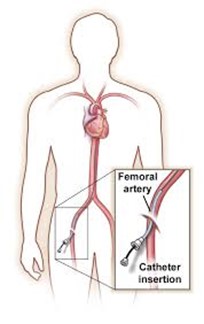
Angiogram
- Magnetic Resonance Imaging (MRI scan): An MRI scan is used to make a detailed picture of the DAVF and its position in the brain in relation to other important structures and is used to plan management/treatment options. If it is close to important (eloquent) parts of the brain for example vision, movement or sensation then a functional fMRI scan may be taken to map the pathways of these structures in relation to the dural fistula
TREATMENT:
Following assessment and scans your care is likely to be discussed by a team of doctors including your neurosurgeon and an interventional radiologist as well as specialist neurovascular nurse. This is called your multidisciplinary team (MDT). They will have an MDT meeting to look at the images gained of your brain and DAVF and make a decision on the best course of management for you.
This decision will take into account your wishes and will ultimately be made by prioritising your safety.
The outcome will depend on the type of DAVF, its position in your brain, its size and how it is affecting you as well as the risk of bleeding. It will also take into consideration your current physical wellness, other illnesses and any risk factors to treatment, for example an unstable heart condition.
There are a number of options for treatment or management to consider: -
These include surgery, endovascular procedures, radiosurgery, a combination of treatments or watch and wait.
The risks of treatment are considered to be high for dural fistula that are located in deep parts of the brain or with very important functions nearby.
Unfortunately, some cannot be treated as the risk is too high. If this is your plan, you will be monitored with scans.
Endovascular treatment:
Endovascular treatment is done by a consultant doctor called an interventional neuroradiologist. This is a procedure similar to an angiogram, but more involved and longer and so you will be asleep under a general anaesthetic. A catheter or catheters are introduced through an artery in one or both legs and sometimes a vein in addition. The catheters are then guided into or near the fistula. Through these catheters, different agents such as metal coils, plastic particles, glue-like substances, and occasionally stents or other devices are delivered to the fistula to selectively close it.
After embolisation If you are well, you are likely to go back to your ward to recover. If you need close monitoring or blood pressure management, you may go to the intensive care unit.
As soon as you feel able, you can go home although you will need a further MRI scan and/or angiogram afterwards to check on progress of treatment.
Depending on the complexity of the dural fistula, embolisation may be done in one stage or more.
If you have a number of embolisation treatments it is worth remembering that each one may affect you differently. You may feel very well after one or experience headaches or symptoms after another. Symptoms, if present, generally settle down.
Surgery:
Whilst you are asleep under general anaesthesia, your neurosurgeon removes part of your skull temporarily to gain access to the brain and the dural fistula. With the help of a high-powered microscope, the surgeon disconnects the dural fistula or closes it off using a titanium clip. The skull bone is then re-attached and the incision in your scalp is closed.
The cure is immediate and permanent as long as the DAVF is closed off completely.
Following surgery, you may go to the ward afterwards to recover. If it is a more complicated procedure, you may go to the Intensive Care Unit for close monitoring and to manage symptoms and control blood pressure. Once you are stable you will go back to the ward for further recovery.
You will usually need a follow up angiogram to check it is occluded. This is usually 3-6 months after.
Open surgery for a DAVF
Stereotactic radiosurgery (SRS):
Without entering the skull, SRS directs many highly targeted radiation beams at the dural fistula to damage the blood vessels and cause scarring. The scarred blood vessels then slowly clot off following treatment. Radiosurgery takes about 2 years to work although may take up to 4 years.
Treatment planning for stereotactic radiosurgery includes a team discussion with the experts in the national radiosurgery unit based in Sheffield.
Conservative management:
Conservative management (“watch and wait”). This will be the option if the DAVF is not thought to be a type that requires treatment.
Conservative management will also be the choice if the treatment risk is higher than no treatment after careful consideration by the skilled medical team. It may also be the choice if your physical health makes the risk of anaesthesia and treatment too risky to be safe.
Risks of treatment:
There are risks to any treatment whether this be endovascular, surgical, radiosurgery or watch and wait: The risks are dependent on the treatment choice, the size and nature of the DAVF and your own physical well-being. These risks (as well as the benefits) will be discussed with you before you make a decision regarding treatment
After you treatment:
After your treatment, once you are up and about and stable you can go home. Your stay may be longer if you have been unwell from a bleed or need rehabilitation either as an inpatient in the Walton Centre or one of the rehabilitation hospitals.
If your DAVF has bled, you have had surgery, or treatment was complicated, expect a recuperation period of up to three months (sometimes longer) off work depending on how you are and the type of work you do.
Recovery varies according to whether you have bled from the dural fistula and any after effects of the surgery and may be shorter or longer according to how well you are.
Rehabilitation:
If you need rehabilitation this will be specific to what is available in your local rehabilitation centre, or what the specialist team think will benefit you most. It includes physiotherapy, occupational therapy, speech and language therapy, dietetic review of your nutrition and psychology.
It may include:
- Specialist inpatient rehabilitation
- Referral back to the hospital you came from for specialist stroke rehabilitation
- Inpatient therapy in the Walton Centre and home with support of local outpatient specialist rehabilitation if needed.
Follow up:
You will be seen in clinic after 2-3 months.
A follow up MR scan and/or angiogram will be recommended once you have recovered to confirm the dural fistula is completely treated. Once you have confirmation that the fistula is gone, the medical team may advise you don’t need further follow up or occasionally wish to review it by scanning after a period of time.
Recovery:
Recovery is individual to each person. It is often quicker if you have never had symptoms or minor symptoms from the dural fistula and when treatment is straight forward.
No matter how well you feel it is worth taking some time (for example a few weeks) to look after yourself after treatment if you are able. This would include time off work if you are able and enlisting the support of family or friends.
If you have bled or have experienced severe symptoms from the dural fistula, recovery will often take longer depending on how this has affected you. After any injury to the brain, most of the recovery takes place in the first six months although it can take up to two years. In certain cases, individuals are left with long term problems such as weaknesses to parts of the body, problems with vision, speech, cognition or epilepsy.
If there are any concerns or problems you will need assessment and rehabilitation from physiotherapists, occupational therapists and speech therapists whilst you are in hospital. This is to make sure you will be safe at home as well as supporting your independence and recovery.
There are occasions a longer period of further rehabilitation is needed in a specialist unit which may delay going home.
Support can be enlisted from clinical psychologists in rehabilitation or as an outpatient as the whole events surrounding the dural fistula can be traumatic and on-going for some.
Information if you have bled or have had effects from the dural fistula:
You will need to pace yourself for the first month; often more after going home because of tiredness and possibly headaches. Save your energy for the things you have to do and those you want to do. Looking after yourself in the early days of recovery is beneficial to your well-being in the long term. You may benefit from gentle exercise as well as a short rest each day in the early days of your recovery.
Feelings of anger, frustration and sadness are not uncommon following a brain haemorrhage. This may be due to the condition but could just as well be due to the sudden life changing event and usually passes with time. If you are affected, you should talk to your GP or neurovascular nurse as you may benefit from being referred (or self-referring) to counselling or a psychologist to help you through this stage of recovery.
Enlist the support of your family and friends whilst you recover. They will be a great help with shopping, transport and support and will be the biggest influence in your successful recovery.
It is advised to have someone stay with you for the first week or so after going home.
Information if you have had seizures:
If you have had a seizure you may need specialist management. One seizure does not count as a diagnosis of epilepsy. A diagnosis of epilepsy is usually made by a specialist neurologist who will manage these symptoms, often through medication.
For your peace of mind and safety, you and your family need to be educated on how to manage the types of seizures you have and what to do if one occurs at home. Information is available for all patients who have epilepsy or have had seizures. This would be through your ward staff, the epilepsy nurse specialist team or the neurovascular nurse specialist team.
The epilepsy nurses give a great deal of support including a dedicated phone line. Advice is also available through Epilepsy Action.
Living with a dural fistula:
Symptoms are specific to each person. You may find that many symptoms are made worse if you are tired, under stress or ill. This is particularly so if you experience seizures, headaches or have bled from the DAVF. People with large DAVF’s that can’t be treated also experience this.
Factor this into your recovery as you may need to look after yourself a bit more or ask for some help during these times.
Lifestyle is important when recovering. Lifestyle choices can make you feel worse or better.
Gentle exercise as you are able, eating well and preventing dehydration all help symptom control. Getting the right amount of sleep helps; too much or too little sleep can make you feel worse.
If you do too much, you may feel worse that evening or the next day. The general rule is if you want to do something and feel able to, then you can. If you find a lot of activity makes you exhausted or worsens your symptoms, then plan an easy day afterwards.
Memory problems:
Memory problems are common in people with dural fistulas. If you have had a haemorrhage from it you may be left with minor or major problems with your short-term memory, attention and concentration. A lot of people report poor memory, even if they haven’t had a bleed. This may be due to changes in blood flow or made worse by worry.
Visual problems:
Visual problems can occur in some cases. These can present as blurred, double, partial or very rarely, complete loss of vision. Assessment and help if you have visual problems can be gained through a specialist eye doctor called an ophthalmologist.
Noises in the head:
Certain types of dural fistula can cause noises such as pulsating or whooshing due to the blood flowing through it.
If the noise gets worse or stops you should contact your doctor or the hospital urgently.
Extreme tiredness:
You will probably need rest once you get home particularly if you are having a lot of visitors or your house is very busy. Even simple tasks such as a walk to the local shop may leave you feeling exhausted. This will improve with time. You will know if you have done too much as you will be exhausted and may experience more headaches. This often happens early evening or the next day and means you have to take a rest! Pacing activities as well as regular exercise will help.
Headaches:
Headaches are common and can persist. If your headaches started after a bleed or treatment, they may ease with time. Headaches can be triggered by dehydration, stress, illness, too much or too little sleep and missing meals. Drinking 2 litres of water a day should help reduce the frequency and severity. Also, try and get back to a normal sleep pattern as soon as possible. Try putting some structure into your day, including meal times as this will help with headaches and recovery. Stopping smoking and reducing the amount of caffeine you take may help reduce the severity of headaches. Menthol sticks to rub on the forehead can help. Drinking a pint of water at the start of a headache may also help. If headaches persist and are troublesome you may need specialist management. This is particularly so if you are still taking regular pain medication after a few months.
Everyday activities:
Driving:
You must not drive, and you must inform the DVLA if you have been diagnosed with a dural fistula. This is even if it hasn’t bled. This is because driving involves many different cognitive and physical skills as well as multi-tasking, decision making and problem solving.
Driving restrictions are enforced by the DVLA and each case has to be approved individually. You must speak to your medical team or nurse to clarify driving restrictions.
Sport and swimming:
Extreme exercise and contact sports should be avoided until the DAVF has been proven to be obliterated and you feel fully recovered. That being said, exercise is encouraged as it improves stamina and wellbeing. Most sports that aren’t extreme or involve contact can be resumed once you feel able and any wounds have healed. You should build up your fitness slowly as you feel able.
If you have seizures you may need to be careful about certain exercise such as swimming. Taking a companion and letting the lifeguard know is advisable if you have had seizures or for the first year after a bleed from an AVM.
Flying:
Flying is not advised in the first six weeks following surgery. You should inform your holiday insurance company that you have a DAVF
Returning to work:
This depends on the job you do, how you are and whether you need a car to work. Most people benefit from some time off to recover and look after themselves. It is advisable to go back to work on a phased return. The length of time you need to recover is dependent on what has happened and what treatment you have had. Your neurovascular nurses will advise you. “Access to work” will support you returning to work if you have a disability.
Washing and dying hair:
You can wash your hair with mild shampoo after 3 days following surgery, but you cannot dye it until the wounds have fully healed and the hair has grown a few cm’s.
If you have had an embolisation procedure, you can wash and dye your hair as soon as you wish.
If you have had stereotactic radiosurgery then you can wash your hair with mild shampoo as soon as you are able. It is advisable not to dye the hair if there are patches of hair loss; you can dye it once the hair has regrown.
Alcohol:
It is best to limit alcohol and adhere to government guidelines. If you experience seizures, there is a risk of provoking one if you drink too much. If you are taking medication, you should check with your doctor if it is safe to drink alcohol.
Illicit drugs:
We recommend that you do not take illicit drugs such as cocaine and amphetamines. As well as being illegal, these can artificially increase blood pressure for long periods of times which isn’t recommended.
Sex:
You can have sex as soon as you feel able.
Pregnancy:
If treatment is planned it is better to wait until after the DAVF is treated before planning pregnancy.
If you become pregnant with a DAVF, then we would recommend that the second stage of labour isn’t prolonged. Your obstetrician may want to speak to your neurosurgical consultant with regards to this so that they can plan a safe delivery for you and your baby.
Home information:
Name: ………………………………………………………….
Consultant: …………………………………………………….
Treatment and date of treatment: …………………………………………………………………….
Follow up:
ADVICE FOR PATIENTS WHEN GOING HOME FOLLOWING ANGIOGRAM:
If the problem is considered serious, help should be sought from your local accident and emergency department immediately. Otherwise, you should contact your G.P., NHS direct or visit your local walk-in centre. `
- Do not strain or lift anything greater than 10lb for 10 days following angiogram
- Drink plenty of water or juice 24 hours before and 24 hours after the angiogram to prepare the kidneys and flush the dye from your body (about 2 litres or 10 glasses)
- Do not drive or operate machinery for 24 hours following angiogram
- Do not do any physical exercise or sexual activity for 24 hours following the angiogram.
- Keep the dressing on, clean and dry for 24 hours following the angiogram
- After 24 hours the dressing can be removed and a shower (not bath) can be taken. A bath and swimming is allowed once the site is fully healed.
- Clean and inspect the site and wash with mild soap and water. Dry and re-cover with a plaster until it is healed completely
- Report to A+E if the site bleeds and not stopped after 15 minutes of firm (but not excessive) manual pressure.
- Report to your doctor/ us/ A+E depending on the severity if there is any swelling; change in colour (paler or darker); change in temperature or change in sensation to the leg/hand.
- Report to your doctor if there are any signs of infection such as redness, pain, swelling or pus from the site.
- Report to your doctor/ us/ A+E depending on severity if there are signs of excessive new bruising (a small amount of bruising is expected from the procedure).
- If you have a new lump in at the site of the angiogram puncture which pulsates you should cover it- do not mobilise and must have it seen to urgently: either go to A+E or inform us
- If you have had a puncture in the groin and develop pain in the abdomen (flank) on the side of the angiogram you must attend A+E or speak to us urgently
Walton Centre Contact Details
For any medical problem or emergency see your G.P or your go to your local Accident and Emergency Department
For information regarding appointments or DVLA forms please contact your consultant’s secretary.
Patient Experience Team provides a PALS service.
0151 556 3090
Neurovascular Nurse Specialists: (practical advice)
0151 556 3325 (answer phone).
Walton Centre switchboard - 0151 525 3611
Useful Contact details
NHS 111: 111
Telephone advice if you need urgent medical help fast but it is not a 999 emergency (or you do not have a GP)
Website: http://www.nhs.uk and search
‘emergency and urgent care’
D.V.L.A. Driver Vehicle Licensing Authority,
Drivers Medical Group, DVLA, Swansea, SA99 1DL.
Medical Enquiries: 0800 032 5202
The Brain Charity: 0151 298 2999.
www.thebraincharity.org.uk
Offers practical help, emotional support and social activities for people with neurological injury. And their families/carers
Stroke association: 0303 3033 10000www.stroke.org.uk
Offers practical help, advice and local support groups
Headway: 0808 800 2244
Headway.org.uk
Offers support to improve life following brain injury
Brain Haemorrhage Support Group: bhsupport.org.uk or through Facebook.
Epilepsy Action: 0808 800 5050
Offers practical help for people who have seizures
NHS Free smoking helpline: 0800 0224 332 www.nhs.uk/smokefree
England: 0300 123 1044 Wales: 0800 085 2219
Advice on Alcohol: www.drinkaware.co.uk or www.drinkingandyou.com
- Last Updated:01 April 2023
- Review Date:01 April 2026
- Author:Catherine Stoneley/Richard Pullicino
- Summary:
WHAT IS A DURAL ARTERIOVENOUS FISTULA?
- It is one or more abnormal connections from an artery supplying the dura of the brain to a vein or venous sinus draining it. The abnormal connection (s) is/are called fistula.