Endoscopic Third Ventriculostomy
You have been diagnosed with a condition called hydrocephalus. This information booklet aims to give you and your family a better understanding of hydrocephalus. Your neurosurgeon has decided that you need an operation to treat your hydrocephalus and an Endoscopic Third Ventriculostomy (ETV), may be suitable. This booklet aims to give you some general information about ETV and its use in treating hydrocephalus. Your doctor will discuss individual treatment options with you, so that you can make an informed decision regarding your treatment.
Your health care team can answer any individual questions you may have and SHINE (Spina Bifida, Hydrocephalus, Information, Networking, Equality) is a national charity, who can provide advice and support should you need it.
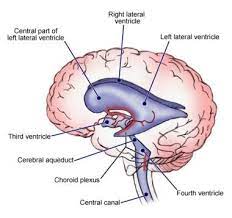
(The ventricular system)
What is hydrocephalus?
Hydrocephalus is a condition in which there is a build up of fluid within the fluid cavities in the brain. The fluid cavities are called ventricles, there are 4 in total. Cerebrospinal fluid (CSF), a water like liquid, is continuously made by and moves through these ventricles. This fluid (CSF) is reabsorbed back into your bloodstream when it reaches the subarachnoid space. This space is one of the layers of the covering of the brain and spinal cord. Hydrocephalus is sometimes referred to as “ water on the brain”. This can occur when the brain makes too much fluid (CSF). More commonly it occurs because the brain cannot absorb this fluid adequately. This can happen for two reasons:
- If there is a blockage of the pathways within the brain preventing the fluid (CSF) reaching the surface of the brain where it is reabsorbed.
- When there is a failure in the brain’s ability to absorb the fluid (CSF) produced.
What causes hydrocephalus?
Hydrocephalus is caused by the body’s inability to drain CSF away into the bloodstream. It can be congenital or acquired. Hydrocephalus is a group of conditions with different causes and the treatment should be given according to cause.
Why does hydrocephalus need treatment?
Some forms of hydrocephalus require no specific treatment, however most forms require treatment and this usually involves surgery. It is important to note that left untreated, hydrocephalus can cause severe problems with memory, concentration, coordination, eyesight and headache. It must be stressed that the effects of hydrocephalus will vary from one individual to another.
How is hydrocephalus diagnosed?
Hydrocephalus is diagnosed using CT or MRI scans.
How is hydrocephalus treated?
There are different treatments dependent upon the cause of your hydrocephalus. The usual form of treatment is to insert a shunting device.
Shunts
A shunt is a device which diverts the accumulated CSF around the obstructed pathway and returns it to the bloodstream. A shunt consists of a system of tubes with a valve to control the rate of drainage and prevent back flow of the fluid. It is inserted in theatre. The upper end is in the ventricle of the brain and the lower end in the peritoneum (abdomen) The device is completely enclosed within the body.
Endoscopic Third Ventriculostomy (ETV)
The surgeon uses a tiny camera called a neuroendoscope to create a hole in the floor of the third ventricle to allow the fluid (CSF) which has built up to reach the surface of the brain. This produces a bypass or shortcut by which the fluid (CSF) can divert past the obstruction to be absorbed normally.
ETV can treat hydrocephalus without the need for a shunt by providing a natural internal pathway and normal absorption of CSF. There is therefore less potential for needing future surgery due to infection or malfunction, as there is no implant left within the body to cause these problems. Less than 1 patient in every hundred will develop post operative infection . Equally symptoms of over drainage are not seen.
If an ETV is to fail it is often within the first few days and up to the first 3 months. However the procedure can be repeated. If successful after this time it is likely to continue to work, however patients and carers need to be aware of the signs of hydrocephalus, as ETV is not a cure. It is said to be successful in 7 out of every 10 patients who have the operation.
ETV is not a new idea, however developments in scanning and equipment have allowed doctors to better identify patients who are suitable for and will benefit from ETV, and perform safer surgery. However, not all patients are suitable for ETV. ETV will only benefit those patients who demonstrate a blockage in the pathways preventing CSF access to the surface of the brain to be absorbed.
The procedure
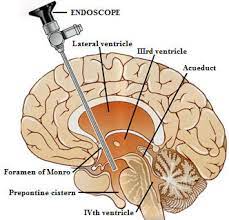
A small hole is made in the skull, usually on the right side and a camera called an endoscope is introduced. The endoscope is then passed through a ventricle, through a narrow connecting channel and into the third ventricle. The floor of the third ventricle is then punctured with a small balloon, which is then inflated to make the hole larger. The endoscope and balloon are then removed. The flow of the CSF keeps the hole open. The operation takes approximately 20mins and there will be a scar of about 2cm, which is usually hidden underneath the hair.
What tests will I need after my ETV?
A post operative MRI scan is usually performed at 6 weeks after surgery, to see if there is flow of CSF through the hole (called the ventriculostomy). However this does not mean the procedure has been successful. The surgeon will also assess your general condition and if you have any signs and symptoms of hydrocephalus.
Does ETV always work?
No, neither ETV or shunt have a 100% success rate. Shunts can malfunction due to blockage or infection. Similarly, the hole created by the endoscope can close, or the surface of the brain may not be able to absorb the diverted fluid (CSF). Hydrocephalus is complex and even though your doctor may be able to make decision based upon assessment of your general condition and the results of any scans or investigations you may have received, he cannot guarantee any procedure.
Your doctor can give you his/her own success rates and those which are documented in the medical literature to enable you to make an informed decision. All operations have some risks. Your doctor will discuss these with you when he/she obtains consent for your procedure.
How do I know if it is working?
Your signs and symptoms will begin to improve or stabilise.
How will I know if it is not working?
ETV is not a cure for hydrocephalus, it is simply a means to manage it. The hole (ventriculostomy) can close. If this is to occur, it can be days, weeks, months or sometimes years after your procedure. It is important that you and your relatives recognise the signs and symptoms of hydrocephalus and seek prompt medical advice if worried. If it doesn't work ETV can be repeated, or other management options such as shunt may be discussed. Your doctor will discuss these options with you.
What if I have a shunt already?
Having a shunt previously does not exclude you from having an ETV in the future. If your MRI scans indicate you have the obstructive form of hydrocephalus, then an ETV may be considered, should a new shunt be needed. However, if there has been a history of infection or haemorrhage (bleeding), this can reduce the chances of success.
What should I expect after my surgery?
You should expect to be a little sore, following your surgery. You will be given analgesia to help with this. You should feel well enough to get up and out of bed the day following your surgery. It is important to do this as soon as you feel able to. You must remember we have changed the way the fluid (CSF) moves inside your head. You may have some dizziness/ lightheadedness when you first get up and out of bed. This is normal. The nurses will assist you as required. You may feel nauseous (sick) or vomit (being sick) after your surgery. You will be given regular medication to help with this (anti-emetics). This is because of the irritation caused by the operation and will pass. Moving around and sitting up in bed will help this pass more quickly. Your wound will have sutures (stitches) or surgical metallic clips closing it. These will be removed after 7-10 days once you are at home. You can wash your hair very carefully, once at home. You will normally be discharged once you are able to get up and out of bed and are feeling well. The time in hospital varies from person to person. You will be given an appointment for a follow up scan post operatively. This is performed at approximately 3- 6 months post operatively. Your consultant will tell you when to expect your scan, before you are discharged home. Contact your specialist nurse team if you have any concerns after you are discharged from the hospital.
Driving
DVLA guidance following this surgery, is that you will be required to notify them and you will be unable to drive for 6 months. After this your license will be reinstated if you are well.
What warning signs should I be aware of?
Any recurrence or worsening of your original symptoms, such as:
- Increasing headache
- Vomiting associated with headache
- New problems with your vision
- ANY leakage from the wound
- Any neck stiffness
- Any raised temperature
- All should be reported to your nurse, consultant or team if you are still in hospital.
If you are concerned once you are at home, please contact us at The Walton Centre.
You can contact the Hydrocephalus Nurse Specialist team on 0151 525 3611 ask for bleep 5340, who can answer any queries or concerns you may have and refer you to the medical staff should you need it.
Reference:
DVLA (2012) Guide to the current medical standards of fitness to drive. Swansea.
Useful addresses
www.shinecharity.org.uk Tel 01733 555988
www.dvla.gov.uk Tel. 0300 790 6801
- Last Updated:01 December 2023
- Review Date:01 December 2027
- Author:Sara Kewin
- Summary:
This information booklet aims to give you and your family a better understanding of hydrocephalus.