Information for Horsley/HDU Critical Care Unit
Welcome to the Horsley ITU/HDU Critical Care Unit
This aims to give simple, practical information to people whose relative, friend or colleague is admitted to our critical care unit. We understand that it is extremely distressing to have someone admitted to a critical care unit and appreciate that you may feel anxious and confused about what to expect. You may have arrived at the hospital whilst their assessment is taking place. It is usual to have to wait during this time whilst the staff organise equipment and stabilise the patient. We realise time can pass slowly and you may feel frustrated by lack of news but as soon as possible a member of staff will talk to you and escort you to see them. The staff are here to help you through this difficult time. Please feel free to ask any questions.
What is critical care?
Critical care is given to patients who are seriously ill and require constant close monitoring in a specialised environment. Patients are looked after by a trained nurse at all times. A doctor is always on duty within the unit and can reach the patient within minutes. Many of the nurses have undertaken advanced courses within critical and neurological care. Patients are admitted to intensive care for close monitoring and advanced airway support, usually requiring ventilation. High dependency patients require more detailed observation or monitoring than can safely be provided on a general ward.
What does the critical care area look like?
The Horsley Intensive Care Unit has sixteen beds, eight in an open main area and eight isolation rooms. The High Dependency Unit has four beds in an open bay. There are no separate male/female sections but every effort is taken to maintain dignity and privacy. Critical care units can be noisy due to the sensitivity of alarms, beeping of equipment and the general everyday activity of telephone rings and staff activity.
Visiting and telephone information
- Horsley ITU 0151 556 3462
- Main desk 0151 556 3541
- HDU 0151 529 5489
The critical care unit is secured by automatic door locks for the safety of patients and staff. On arrival you will need to press the intercom on the wall for either Horsley or HDU and state whom you have come to visit. Please be patient, due to work pressures staff may be busy and take some time to answer the intercom. On entering the unit the waiting area is to your right.
Please do not let any people into the unit without the knowledge of a member of the nursing team
When telephoning for information the nurse looking after a patient has to leave the bed space to take the call. We appreciate that family and friends want to know how the patient is doing, but there is very little information the staff can provide over the phone for reasons of confidentiality. It would be beneficial to designate one or two family members who could ring people to pass on information. The doors to Horsley ITU/HDU are normally locked and you will need to ring a doorbell to gain access. Again, please be patient and wait for a reply. Sometimes the doors are left open for staff to move patients quickly. Please do not enter the unit without speaking to a member of staff.
There is a hand wash basin on the corridor leading to the ITU/HDU, please ensure you wash your hands prior to entering the unit. There are dispensers on the wall near the entrance containing a gel to clean your hands which you must use when entering and leaving the unit.
Visiting on Horsley is 12pm — 2pm and 4pm — 8pm but patients need a lot of rest and close monitoring and there will be times that you will have to wait long periods whilst the patient receives care/treatment.
Please speak to the nurse in charge with any special requests for visiting. The staff will provide on going information and the medical team will speak with you to explain the treatment plan. You may wish to write down any questions that you wish to ask the staff. Two visitors are allowed at the bedside at any one time and,
initially, it is advisable that only close family/friends visit. Visitors will be asked to wear an apron at the bedside and sometimes gloves. Babies and young children should not be brought into the unit due to the risk of infection being passed on to them. Older children may visit but it is best to discuss this with the nurse in charge prior to visiting. Visiting for HDU is from 2pm—4pm and 6pm—8pm, again, only two people at a time at the bedside please. Space is very limited, so we would be grateful if you could take home all property except for essentials like toiletries. Please do not send flowers to the unit and keep hold of any get-well cards until discharged to the ward.
Who are the staff on the critical care unit?
Staff in the critical care unit work as part of a team to provide the highest standard of care 24 hours a day. Each patient has a designated trained nurse to care for them on a one-to-one basis, or one nurse to two patients, this depends on the level of care required.
The nursing staff will be able to provide you with updates and future goals. Senior nurses wear navy blue scrub suits, staff nurses wear light blue and health care assistants wear light grey.
The most senior doctor on the unit is a consultant. Consultants specialise in a particular area of medicine. The consultants based on the unit are anaesthetists. Consultants are assisted by other doctors called registrars, fellows or senior house officers. A consultant surgeon will be looking after your relative/friend, or a consultant neurologist will also be involved liaising with the consultant anaesthetist, to ensure the best possible care.
Physiotherapists visit the unit to help treat a patient’s chest. Many patients are at risk of chest infections because their lungs are not functioning well enough to prevent a build up of secretions. Physiotherapists are also involved in rehabilitation and limb exercises.
The pharmacist is involved in monitoring the effects of medicines on patients and ensures the supply of all necessary drugs.
A radiographer will visit to take portable x-rays.
The dietitian ensures that each patient is receiving enough calories and nutrition.
A microbiologist is involved in monitoring the risk of infection and advising on appropriate treatments.
The Critical Care SMART Team
Patients are usually transferred from the critical care unit when they are able to breathe on their own and no longer need specialist skills and equipment. The Walton Centre is a specialist regional hospital and once the patient no longer needs specialist care it is common to transfer (repatriate) patients back to the original hospital that they came from. Many families feel anxious at this time. Once the patient is ready for transfer from the critical care environment to our wards a member of the SMART team will be informed. The SMART team operates a multidisciplinary approach comprising both nursing and medical members led by a Specialist Nurse and supported by senior medical staff. Their role is to support and assess patients on discharge from the critical care area throughout the hospital. They particularly support the more highly dependent ward patient and those who require tracheostomy care. They will review your relative within 24 hours of discharge from critical care, and further support until their input is no longer needed.
What does all the equipment do?
The initial reaction on entering an ITU for the first time can be overwhelming. Machinery, alarms, tubes etc. We would like to simplify the functions of the equipment with these short explanations. A ventilator is a machine that assists a patient’s breathing. It pushes air into the lungs via a tube (endotracheal tube) that is placed into the windpipe via the mouth or nose. The ventilator can either “breathe” completely for the patients or it can be set to assist in the patient’s own breathing.

A patient cannot speak whilst on the ventilator and they will need regular suctioning via the endotracheal tube to remove secretions, this may make them cough.
All patients are attached to monitors, which are like TV screens that constantly provide the staff with information such as heart rate, blood pressure, oxygen saturation as will as other specific needs. These are very sensitive and can alarm to alert staff to changes on the monitor.

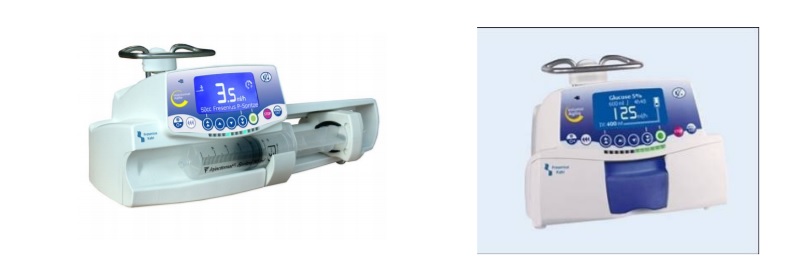
All patients have various drips attached to their body to provide hydration as well as infusing all the necessary drugs, such as sedation and pain killers, to ensure that they are comfortable. Please feel free to ask a member of staff about any of the fluids. Patients regularly need to go for scans to assess their condition and plan care.
Your relative/friend may look different due to all the equipment and nature of their illness and it is understandable that you will feel anxious about what to expect.

The nurses are here to support you through this difficult time. Please feel free to talk to your loved one to let them know you are there and don’t be afraid to touch them. Patients who are likely to be ventilated for over 48 hours will have a diary to help them understand what happened to them whilst in intensive care. We would encourage you to write in the diary any news from home, messages of support and who has been visiting. This helps greatly in the recovery process.
If you would like to be involved in any care such as bathing, please tell one of the staff. You are certainly under no obligation to help but doing so can often bring some comfort.
The risk of pressure ulcer development in the critically ill patient
A pressure ulcer is damage to the skin and the deeper layer of tissue under the skin. This happens when pressure is applied to the same area of skin for a period of time. Pressure ulcers can develop on any area of the body, but generally occur over bony areas, for example; the back of the head, heels or sacrum. Pressure ulcers can also be caused by medical devices used to monitor the patient’s condition or provide essential treatment. Sometimes adhesive tapes used to secure devices may also irritate susceptible skin. In most cases pressure ulcers are avoidable, however in a few cases, they may be deemed as unavoidable, for example, the patient may be considered too ill to move, or the device causing damage may form a key element in the patients treatment. Every possible precaution will be taken to prevent it with the use of pressure redistribution aids and devices removed as soon as is possible
Those patients who are at particular risk are those who are critically ill, over 70 years of age, immobile, incontinent (trouble controlling bladder or bowel function), or who have sustained serious trauma.
Facilities at The Walton Centre
There is a café and cash machine located at the main entrance and larger dining room situated in Aintree Hospital, across from the Walton Centre. Staff can give you directions to there and also to local shops, bus stops and train station, just ask for any help you need. A toilet is located inside the visitor’s waiting area and also in the main entrance. Please turn off your mobile phone whilst on the unit. Taking photographs is not permitted. Please do not make comments about patients on social media sites (Facebook etc), please respect patients confidentiality.
The visitor’s room is provided for the use of relatives of patients on the Horsley Intensive Care Unit and the High Dependency Unit. Because it has to serve a large number of people there are no facilities for using the room for sleeping purposes as this restricts the use for other people. You are welcome to stay overnight, if this is necessary, but we would remind you that this is a sitting area and furniture should not be re-arranged for purposes of sleeping.
Support and advice
- Religious representatives of various denominations visit the hospital.
- Please inform the staff if you would like to speak to one or make arrangements for your own religious representative to visit. There is a multi-faith room located on the first floor which you may like to use. Please ask staff for directions.
- Medical certificates can be obtained by speaking to the nursing staff.
- Patient Experience Team provide confidential impartial help and advice to families/visitors. Tel 0151 556 3090/3091 (9am - 5pm) Monday - Friday.
Headway Acute Trauma Support (HATS) nurses provide support, information and advice for families of people with brain injury. Website www.headway.org. Helpline 0808 800 2244. - ICUsteps is a registered charity set up by former ICU patients and their relatives that provide information and support. Website www.icusteps.org.
- Parking information: https://www.thewaltoncentre.nhs.uk/contact-us/directions-and-car-parking.htm. Not to be used in Aintree Hospital car parks.
We hope this booklet has provided you with enough information at this time. Above all, remember the staff are here to help you and are happy to answer any questions you may have.
- Last Updated:01 September 2022
- Review Date:01 September 2024
- Author:P Stone
- Summary:
This aims to give simple, practical information to people whose relative, friend or colleague is admitted to our critical care unit.