Intraventricular Haemorrhage
What is an intraventricular haemorrhage (IVH)?
This is bleeding inside the ventricles which are the fluid compartments of the brain
The blood can just be within the ventricles (primary) or it may also extend and involve the brain itself (secondary).
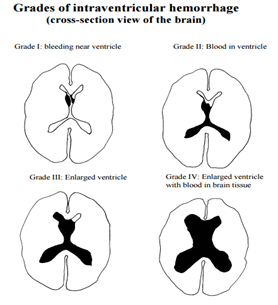
(Grading for intraventricular haemorrhage is more commonly done for babies but this picture gives an example of where the bleed is)
What causes intraventricular haemorrhage?
There are a number of causes of IVH including
- Aneurysms or vascular malformations of the blood vessels in the brain
- High Blood pressure (hypertension)
- Other vascular malformations close to the ventricles of the brain
- There are other more rare causes or sometimes no cause is found after extensive investigations
- Sometimes no cause is found
Diagnosing an intraventricular haemorrhage:
This is usually made by your history and head scan (CT scan).
If the tests appear positive, you will be transferred to the Walton Centre for further investigation.
You will be given regular pain killers and medication to help prevent sickness. Laxatives will also be offered as the pain killers can cause constipation.
You are usually required to stay hydrated: This is either by drinking or by a “drip” into the vein. It is important your urine output is measured every time you go to the toilet. Plenty of fluids help keep a good blood flow to the brain.
If it is thought that the cause of the bleed in from an aneurysm you will be given a 21-day course of tablets called Nimodipine. These have to be taken every 4 hours and help prevent complications due to haemorrhages from an aneurysm rupture.
Investigations to find a cause
- You will undergo a brain scan after injection with contrast which shows the blood vessels within the brain. This is called a CTA (Computerised Tomography Angiogram) and is used to detect blood vessel abnormalities that may have caused the bleed.
- If the CTA is negative, and after the doctors review your case, you may require a more formal angiogram called a DSA (Digital Subtraction Angiogram). This is a test which involves the injection of dye through a catheter (tube) inserted into an artery in the groin or wrist which is then passed up to the brain through major blood vessels and a series of x-ray pictures are taken. This shows very clear pictures of the blood vessels within the brain. You may be given provisional results immediately but formal results are given once these pictures are reviewed in depth by your medical team. There is a separate information leaflet regarding the angiogram which you should get when you sign consent.
- If a cause is found then your team will discuss ongoing management. The type of treatment will be decided depending on what is found and varies according to the cause. If a cause is found; this will be discussed with you and there are separate information leaflets to address the various causes.
No vascular abnormality Found
If no vascular abnormality is found, your case will be reviewed by a panel of experts called the multidisciplinary team.
They may advise delayed investigations for when the blood has reabsorbed which can take some time.
When no cause is found, no treatment will be required other than to support you through your illness by managing symptoms and lifestyle factors such as blood pressure control.
Whether a cause is found or not you will still need to recover from the bleed itself.
Further Investigations
In certain cases further tests are necessary. These are specific to each individual case. They may include further tests such as an MRI scan either whilst you are in hospital. It may be decided you need a delayed angiogram or an MR scan of your brain as an inpatient or after you go home.
External Ventricular Drain (EVD)
There is a risk of build up of fluid within the fluid compartments of the brain after an intraventricular bleed: This is called hydrocephalus and can be life threatening because it can cause an increase of pressure within the brain.
If this occurs, an external ventricular drain may be needed. This is a temporary thin plastic tube which is inserted to drain the fluid within the brain (cerebro-spinal fluid).
Because the hydrocephalus is caused by blockage of the reabsorption of brain fluid (cerebro-spinal fluid) by the haemorrhage then in most cases it settles down as the blood is naturally reabsorbed and the tube can be assessed and removed with time.

Shunt
In some cases a permanent diversion tube is needed called a shunt
This is an enclosed tube which drains the brain fluid (cerebro-spinal fluid) from the brain to the abdominal cavity where it is reabsorbed into the blood stream. It is completely enclosed within the body and sterile. They usually stay in for life. There is a separate information leaflet about shunts available and you will be supported by the hydrocephalus nurse specialist’s when you go home if you have one.
Going home
Once it is decided that no further investigation is needed as an inpatient and your medical team are happy that you are recovering you will be allowed home.
You may need further investigations as an outpatient. The tests you will need should be discussed with you before you go home.
It is advised that you get your blood pressure, renal function (kidney function) and cholesterol checked by your GP after going home. Your blood pressure should be monitored regularly and kept under control within normal guidelines that your GP will be aware of (NICE guidance).
Medication
Hypertension (blood pressure) medication:
You may go home on medication to control your blood pressure; if this is the case, you should make an appointment with your GP when you get home to have your blood pressure monitored and the medication adjusted if needed.
At that time you should also have your kidney function checked (renal function) as high blood pressure can sometimes reduce renal function.
Pain Relief
You may go home with pain killers. You should take these regularly to begin with if you need them. They should be cut down as soon as tolerated as taking them for too long may make headaches worse not better!
Certain types of pain killers can cause constipation and so laxatives are usually given to you. Eating a diet that is high in natural fruit and fibre helps too.
If medication side effects occur, seek medical advice.
Recovery
You will benefit from a regular routine in the early days of your recovery; This means keeping hydrated: going to bed and getting up at the same time and not missing meals as well as pacing your activities and taking some outdoor exercise such as walking.
Your recovery will also benefit from getting as much help as you can in the early days although you should aim to be gradually more independent as you recover as some people will lose confidence because of the sudden and life-threatening nature of this illness.
Limit visits to a about an hour if you are feeling tired but still take time to enjoy your family and friends as they will be a big support for you.
Recovery is dependent on how you feel.
You will need to pace yourself for the first month or more after going home because of tiredness and headaches. Save your energy for the things you have to do and those you want to do.
Looking after yourself in the early days of recovery is beneficial to your well being in the long term.
Feelings of anger, frustration and sadness are not uncommon following an intraventricular haemorrhage. This may be due to the condition but could just as well be due to the sudden life changing event and usually passes with time and support. If your mood is low, you lose confidence or find yourself becoming more socially isolated, you should talk to your GP as you may benefit from being referred for talk therapy or a psychologist to help you through this stage of your recovery.
You will be given some leaflets and information to support your recovery before you go home – please speak to your neurovascular nurse specialist.
Extreme tiredness
You will probably need rest once you get home particularly if you are having a lot of visitors or your house is very busy. Even simple tasks such as a walk to the local shop may leave you feeling exhausted. This will usually improve with time although doesn’t always completely go away. You will know if you have done too much as you will be exhausted and may experience more headaches. This often happens early evening or the next day and means you have to take a rest!
Pacing
You may benefit from pacing your activity for the first 4 weeks or more if needed following going home. Take some gentle exercise. Build up activity as you feel able to and try to go outside for regular walks if you are able; otherwise you may lose your confidence and fitness which may then affect your recovery and well being. Aim to build up to half hour walks 5 days a week if you can. You will probably need to take a rest each afternoon in the first few weeks of recovery.
Unusual sensations
Some people experience unusual or strange sensations in their head following a brain haemorrhage. These are common symptoms and we are not sure why they occur. Do not worry about them as they should ease with time. If you are unsure of these symptoms, please discuss with your neurovascular nurse specialist.
Sensitivity to noise
This is not uncommon following a brain haemorrhage. Everyday and loud noises noise such as television or background conversations can be just as difficult to cope with as your brain is recovering. This usually settles down with time as you recover and learn to cope with the ongoing symptoms of your haemorrhage
Headaches
Headaches are common after any brain bleed and usually they usually ease with time. They may, however, persist. Headaches can be triggered by dehydration, stress, illness, too much or too little sleep and missing meals. Prolonged or regular use of analgesia (paracetamol, ibuprofen, codeine, morphine etc.) may also worsen or prolong headaches so should be used sparingly and stopped if no longer required. Drinking 2 to 3 litres of water per day, regular meals, ensuring a good sleep pattern and in some instances avoidance of certain triggers (caffeine, alcohol, cheese etc.) can help reduce the frequency and severity of headaches. There are also some non-invasive treatment options such as menthol sticks to rub on the forehead which may help. Drinking more water and using pain relief at the start of a headache may also help. If headaches persist and are troublesome despite this, you may need specialist management.
If your headaches persist or get worse, seek advice from your GP.
Fear of re-bleed
This is a very common fear for all patients, particularly if no cause was found. The chance of another bleed is extremely rare and is usually no higher than everyone else in the general population.
It is important to learn a coping strategy as this fear may prevent your recovery progressing. You can do this through talking therapy with a counsellor. You can usually self-refer to a local counsellor online or by calling them.
In the unlikely event that you get the same symptoms as you did when you had a brain haemorrhage you will need to go to your local accident and emergency department.
Family and friends
Enlist the support of your family and friends whilst you recover. They will be a great help with shopping, transport and support and will be the biggest influence in your successful recovery.
It is advised to have someone stay with you for the first week or so after going home.
The “Brain Haemorrhage Support group” affiliated to the Walton Centre also offer emotional support and practical (not medical) advice from personal experience (details in the back).
Everyday Activities
Driving
You should not drive following brain haemorrhage until you have recovered and received the go ahead from the DVLA.
This is because driving involves many different cognitive and physical skills as well as multi-tasking, decision making and problem solving.
DVLA guidance changes all the time and so please check the advice available on the direct .gov website
You cannot drive if you have had an EVD or shunt insertion for at least 6 months and must inform DVLA
You cannot drive if you have new visual problems, cognitive problems or stroke like symptoms.
You cannot drive if you have had a seizure (or fit) as a result of the intraventricular haemorrhage (this is likely to be a year since the last seizure).
Driving restrictions are enforced by the DVLA and each case has to be approved individually. You must speak to your medical team or nurse to clarify driving restrictions.
Returning to work
You can return to work as soon as you feel able from about 6 weeks following your brain haemorrhage. It will not make you ill to return sooner if you recover sooner and want to or have to for financial reasons.
Most people, however, need about 3 months or more to recover. (Occasionally longer if there have been significant problems)
You should go back to work on a phased return. This means you build up your working days and hours gradually according to how you are feeling. A phased return is often graduated over 4 weeks or longer and your employer has an obligation to adhere to it.
The Brain Charity will help you if you are having problems with returning to work. The number is printed at the back of the booklet.
Will I be entitled to any benefits?
You may be entitled to sick pay from your employer, or you may be able to claim benefits appropriate to your specific situation. You should contact an agency such as Citizens Advice Bureau or Brain Charity to discuss individual circumstances and what you are entitled to.
Drinking Alcohol
You should avoid alcohol until you are feeling more recovered, and you have reduced the number of pain killers you take. However, most people find they are not able to tolerate large amounts of alcohol.
If you are taking Nimodipine, do not drink alcohol until the 21 day course is completed.
The government suggests no more than 14 units a week. Details of an information website on alcohol awareness is printed at the back of this booklet
Smoking Cigarettes
It is advisable that you give up smoking completely. A free help line number is printed at the end of this booklet.
Sexual Activity
You can resume sexual activity as soon as you feel able.
Starting a family
You can start a family as soon as you have concluded investigation and have results that all is well. You will benefit from taking a few months to recover your physical fitness before planning a family. You will not normally be prevented from a normal delivery, but this will depend on the cause of the bleed and treatment. Your neurosurgeon will advise you and your obstetrician.
Sport and swimming
Exercise is encouraged as it improves stamina and well being. Most sports can be resumed once you feel able. However, you should build up your fitness slowly as soon as you feel able. It is advisable to go swimming with somebody during the first year following your brain haemorrhage.
Extreme exercise should be avoided until all delayed investigations are complete and results have been given.
Dental Treatment
Dental treatment is safe after an intraventricular haemorrhage. Your dentist may need to seek advice from your neurovascular nurse, consultant or GP.
Flying
If you have had an intraventricular with no vascular abnormality found, you should be able to fly as soon as you feel able.
If you have more specific questions please ask your neurovascular nurse specialists, medical team or ward nurses.
Information for self help
- Brain Haemorrhage Support Group offers practical advice and emotional support for all patients and their families/friends that have had brain haemorrhages.
- Brain Charity– Information and support for people with neurological Conditions (Leaflet available at the helpdesk on the ground floor).
- BASIC (Brain and Spine Injury Centre ( Manchester) ( details at the end of this leaflet)
- Information is available for all patients who have had shunts inserted as a result of brain haemorrhage. (Through your ward staff, neurovascular nurse specialist, hydrocephalus nurse specialist.)
- Information is available for all patients who have epilepsy as a result of brain haemorrhage. (Through your ward staff, neurovascular nurse specialist, epilepsy nurse specialist.)
- Access to Work: https://www.gov.uk/access-to-work . This is a government based web site that will advise you on how you can be supported when returning to work
ADVICE FOR CARING FOR PUNCTURE SITE TO GROIN/WRIST POST OPERATIVELY.
If the problem is considered serious, help should be sought from your local accident and emergency department immediately. Otherwise, you should contact your G.P., NHS direct or visit your local walk in centre.`
- Do not strain or lift anything greater than 10lb for 10 days following angiogram
- Drink plenty of water or juice 24 hours before and 24 hours after the angiogram to prepare the kidneys and flush the dye from your body (about 2 litres or 10 glasses)
- Do not drive or operate machinery for 24 hours following angiogram
- Do not do any physical exercise or sexual activity for 24 hours following the angiogram.
- Keep the dressing on, clean and dry for 24 hours following the angiogram
- After 24 hours the dressing can be removed and a shower (not bath) can be taken. A bath and swimming is allowed once the site is fully healed.
- Clean and inspect the site and wash with mild soap and water. Dry and re-cover with a plaster until it is healed completely
- Report to A+E if the site bleeds and not stopped after 15 minutes of firm (but not excessive) manual pressure.
- Report to your doctor/ us/ A+E depending on the severity if there is any swelling; change in colour (paler or darker); change in temperature or change in sensation to the leg/hand.
- Report to your doctor if there are any signs of infection such as redness, pain, swelling or pus from the site.
- Report to your doctor/ us/ A+E depending on severity if there are signs of excessive new bruising (a small amount of bruising is expected from the procedure).
- If you have a new lump in at the site of the angiogram puncture which pulsates you should cover it- do not mobilise and must have it seen to urgently: either go to A+E or inform us
- If you have had a puncture in the groin and develop pain in the abdomen (flank) on the side of the angiogram you must attend A+E or speak to us urgently
- Last Updated:01 October 2023
- Review Date:01 October 2027
- Author:Cathy Stoneley
- Summary:
What is an intraventricular haemorrhage (IVH)? This is bleeding inside or around the ventricles which are the fluid compartments of the brain