Lumbar spine surgery
Admission to hospital can be a daunting experience for most people.
The following information is designed to give you information about your stay at The Walton Centre and what to expect. This information is intended as a guide and may vary depending upon your individual requirements. It also contains your physiotherapy exercises for you to do following your surgery and some general advice following lumbar spinal surgery.
This booklet does not contain information about a specific operation, but the advice, experience and recovery for most patients undergoing lumbar spine operations is very similar. There is an explanation of some terms that may be relevant to you and your surgery toward the end of the page. If you have any questions before or after your surgery, then please contact us via the contact details at the end.
For further information please see patient information on British Association of Spine Surgeons website (spinesurgeons.ac.uk/Booklets) .
How is the spine constructed?
The spine is constructed in two parts, the spinal column which consists of the bones (your back bone) and the spinal cord which consists of the nerves of the spinal cord that pass messages through from your brain to your body and back again.
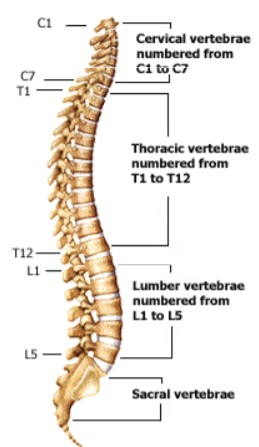
Spinal column
The spine is composed of small bones called vertebrae which all sit on top of each other to form your spinal column. The vertebrae get larger as they go down the spinal column, with the largest being in the lumbar (lower back) region.
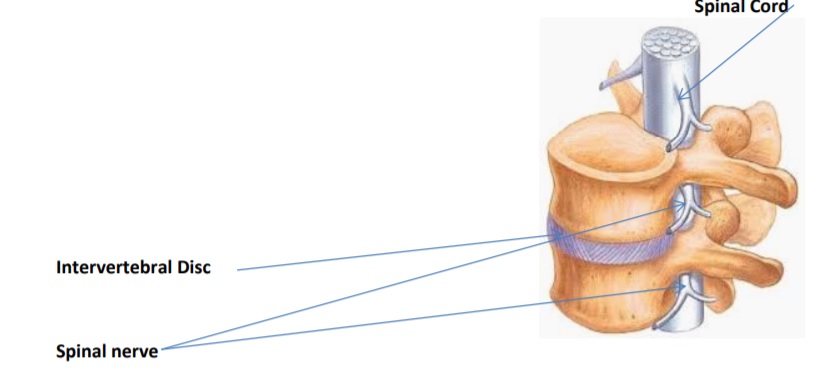
To stop these bones from rubbing on each other you have intervertebral discs. These are soft cushions of tissue, which sit in between each of the bones in your spinal column and act as shock absorbers, stopping the bones from rubbing on each other.
There is a tough band of elasticated tissue called the ligamentum flavum, that helps the stability of the spine by connecting the bones together. The spinal cord and nerves are protected by a thin layer of tissue, called the dura mater, and this contains the fluid, called CSF, that surrounds the nerves and spinal cord.
The spinal column is very strong and flexible and is held in place by many structures. The cervical (neck) and lumbar (lower back) areas are more prone to problems as these are the areas that move the most to allow us to move our head and bend and stretch in the lower spine area.
Spinal cord
The spinal cord consists of millions of nerve fibres which run through the middle of your spinal column. Your spinal cord, and the nerves it is composed of, act in a similar way to a telephone exchange passing information from your brain to your body and back again. At the level of each bone (vertebra) your spinal cord sends out one nerve on the right side and one on the left side. These nerves contain hundreds of nerve fibres that transmit messages between your body and brain.
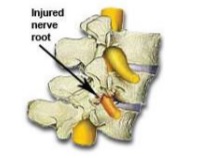
Spinal nerve
The cervical vertebrae are in your neck, thoracic are in your trunk and the lumbar and sacral vertebrae are in your lower back. Any problems with your spinal column that causes pressure on your spinal cord or nerves can cause problems with feeling and/or movement. The nerves in the lower back are responsible for the feeling and/or movement from below your waist, and so any problems in the lower back may result in symptoms in this area. This can include problems with pain, numbness, weakness, or altered sensation due to pressure on the nerves. As we age the spine is prone to degenerative changes which in combination can cause pressure to the nerves or spinal cord.
Pressure to nerves can be caused by one or a combination of factors:
- Slipped disc/bulging disc
- Osteophytes – overgrowths of bone
- Ligaments – elastic tissue,that can become hard and calcified with age
- Enlarged joints – get larger with age, wear and tear
- Non-alignment of the bones – often becomes worse with degenerative changes
Why do we perform spinal surgery?
Surgery for problems with the spinal column or spinal cord and/or nerves, can be performed for many reasons. In general you will have been offered surgery to:
1. Give you relief from pain
2. Stop any further deterioration in the feeling and/or function from below your waist and more often in your legs.
3. Give you a chance of making some recovery from any symptoms.
The main aim of surgery is to remove what is causing the pressure on the nerves (e.g overgrowth of bone, thickened ligaments) and help to improve your pain and leg symptoms (70-80% chance of improvement). It is also important that you understand, that spinal surgery is often performed in order to improve your leg symptoms and prevent any further deterioration in movement or sensation, movement and movement and sensation cannot always be improved.
If nerves and/or spinal cord have sustained damage, quite often over a long period of time; the damage already caused to the nerves or spinal cord may not be reversible, despite surgery to remove the problem. This is why sometimes weakness, numbness and other symptoms may not improve. Any recovery of symptoms will often take time, and can take several months to manifest itself.
Surgery is not for your back pain, and is aimed at your leg symptoms.
The following information is to help you understand what we are offering you and why. Please remember, agreeing to surgery is your decision. The job of our team is to present you with the facts and options as we see them. You have the right to change your mind at any point in time. If you wish for further explanation at any time please just ask one of the staff.
What are the risks?
All the risks will be discussed with you prior to your surgery and although they are not common you should be aware that there is the potential for them to occur
- Risk from anaesthesia (being put to sleep for your surgery), please see anaesthetic book.
- Risks from positioning during surgery and equipment used), this can include skin injuries, eye complications, most severely blindness but this is exceptionally rare. Special gel pads/protection is used during surgery to minimise the risk of these complications. Diathermy pads are used which is an adhesive pad placed on the skin, usually the thigh area, to minimalize heat build up, this can cause skin irritation and in exceptional cases a skin burn.
- Small risk of increased pain in back or leg, or no improvement in leg pain/symptoms.
- Risk of injury to the nerves (less than 1%) and more common in patients having repeat surgery (10%). This can cause weakness or numbness in the legs, and/or problems with the function of the bladder, bowel and sex organs. In the extreme this could mean paralysis from the waist down but this is exceptionally rare.
- Leak of spinal fluid, this is where there is a tear in the lining which surrounds the nerve roots, this occurs in less than one in 100 patients. This is repaired with stitches, a patch or special glue. The worst case scenario is that further surgery is required to repair the leak but this is extremely rare (0.05%) this is more common in repeat surgery. This can cause headaches and sickness, in very rare cases infection in the CSF fluid (meningitis). A leak sometimes needs a further operation to repair this with stitches, glue or a patch.
- Infection, superficial wound infections can occur in approx. four out of 100 patients and are easily treated with antibiotics. Deep wound infections occur in less than one out of 100 patients, but these can require further surgery and long courses of antibiotics. Infection risk includes infection from the MRSA bacteria (infection with MRSA is very rare). Any infection can result in sepsis but again this is exceptionally rare. Those with weakened immune systems, diabetes or taking steroid medication are more at risk of infections from surgery.
- Wound drain problems, requiring removal in theatre, whilst under anaesthetic, which again is very rare.
- Bleeding or haematoma (collection of blood), in very rare circumstances this can require a further operation.
- Risk of deep vein thrombosis (DVT) or pulmonary embolus (PE), The risk is rare and we use special surgical stockings, and blood thinning injections where appropriate to reduce the risk.
- Worsening of symptoms.
Are there alternatives to surgery?
It is your decision if you wish to have surgery and surgery will only have been offered to you if your consultant feels that it may be of benefit to you. If you do not wish to have surgery then your neurosurgeon will discuss the individual implications this will have for you.
Here are some alternatives that may be suggested to you:-
1. Wait to see if your condition remains unchanged without surgery.
2. Manage your pain with analgesia (pain killers)
3. Pain team intervention, to see if they can help manage your symptoms
4. Try conservative measures, for example physiotherapy and/or exercise such as pilates or Thai chi.
Pre-operative assessment
It is important, if you have any changes in your pain or symptoms and also if you develop any new medical conditions or are unwell, you speak to spinal nurses or your consultants secretary at the earliest opportunity but definitely prior to attending for your admission.
In order to gain the information we need to ensure your safety during your surgery, once you have agreed to surgery you will be required to complete a pre-operative assessment online. You will be provided with the information you need on how to complete this. The information you provide will be reviewed by one of the pre op nurses. Once this is done you will be contacted to explain the next steps that will be applicable to you and the procedure you are undergoing.
For some patients you will only need to attend for some blood to be taken for testing, and routine swabs. Some patients will need to be spoken to by phone to clarify medical details, some will need to come in to clinic to be seen and examined.
It is very important that you complete your pre-operative questionnaire with all the details as accurately as possible, as inaccurate information may delay your surgery.
If you do have to attend for an assessment it may include:-
1. A member of the team will discuss your medical history (your past operations and any medical conditions you may be suffering from) with you and you will be examined.
2. You may be reviewed by an Anaesthetist; he/she will have a chat with you and discuss any relevant medical history and explain what having an anaesthetic will involve.
3. You will have some blood tests performed.
4. If any x-rays or a heart trace (ECG) are required these will also be done.
5. Your medication may be prescribed; it would be helpful if you could bring with you any medication that you are taking or a list of your medication and doses. It is very important that you tell us about all your medication, including all prescribed medication, medication you buy and any herbal remedies. It is especially important that you tell us about any medication that may thin your bloods.
An appointment will be organised for you and sent to you if you are required to attend for this.
Some patients may not have a pre-operative assessment of any type, this can be for many reasons, for example, you are admitted urgently or as an emergency and there is no time for all of this to be completed. This is not a problem, because everything you need will be done the day you are admitted. Your surgery in this situation is normally the following day. You will not go home overnight.
Please be patient whilst we complete all of our assessments. It is important that we ensure everything is completed to ensure your safety. Occasionally we need to postpone surgery if your pre-operative assessment indicates that there are more tests or assessments needed before we proceed with your surgery. We understand that this is frustrating, but we will not proceed until we have all the information we require to ensure your maximum safety.
Admission to hospital
You will be able to eat and drink up to midnight the night before your surgery and drink clear water only up to 6am on the morning of your surgery. You will then be able to have sips of water only from 6am until you go for your operation. This will be clarified for you prior to your admission. Most patients will be admitted the day of their surgery at approx. 7.15am, having followed the fasting instructions above.
It is advisable not to bring any valuables with you into hospital as the hospital does not accept any responsibility for their safety. When you arrive you will be seen in an admission area and then informed which ward you will go to after your surgery.
The day of surgery
You will continue to be kept fasted (nothing to eat or drink) and need to wear a theatre gown, we would ask that you have a bath or shower the morning of your surgery before you leave home.
Your details will be checked with you on the ward before you go to theatre. You will be wearing a wrist band and have to answer a list of questions, for example, your name, date of birth and confirm that you have removed all jewellery, underwear and make up etc.
You will be collected for theatre and taken to the theatre reception area, where the Nurse will check your details again; whilst this can appear repetitive it is all done to ensure your safety. From there you will be taken to the anaesthetic room, where your details will be checked again. We have a robust safety check list which includes asking you to confirm what operation you are having, your symptoms, which side of the body and where you experience them, do not be concerned, this is for safety only and not because of any queries about your surgery. Once this is done the anaesthetist will give you your anaesthetic medication, and once you are asleep you will be taken into theatre and surgery performed.
The surgery will be performed by the consultant or one of their team. It is common for x-rays to be used in theatre to assist the surgeon with checking the correct position of the spinal bones and surgical level.
After surgery you will be taken on your bed into the recovery room where you will be monitored whilst you wake up from your anaesthetic, and you will be made comfortable for your transfer back to the ward. You will be transferred back to the ward after spending approximately one to two hours in recovery. On return to the ward your observations i.e. blood pressure and pulse, will be checked regularly, as will your wound and your limb power and movement.
An intravenous infusion (drip) will be in your hand until you are awake enough to eat and drink again. You will be able to have sips of water a few hours after you return to the ward and then increase this as you feel well enough.
You may require a wound drain, this is a small plastic tube located just beneath the skin that comes out of the skin near wound and is attached to a plastic collection device. It drains any excess fluid/blood away from the wound but is not always needed.
If your surgery is early in the day then you should be able to get out of bed and mobilise around the ward the evening of your surgery. Once you have recovered fully from the anaesthetic we will be happy for you to be out of bed.
It is normal to feel some discomfort in the wound area after surgery and around the hip area (due to positioning in theatre) but we will manage this with appropriate pain relief medication.
Some patients will have a PCA (patient controlled analgesia) this is a push button device that allows the patient to push a button, to deliver some pain killing medication into the vein through a small plastic tube with each push of the button. It has a time out switch so that it can regulate the amount of medication delivered. This is often used for the more extensive procedures or where pain control is an issue, and this will be decided on an individual patient basis.
The day after surgery
In most cases the day following surgery your drip will be removed, your wound will be checked and if you have a wound drain, it will be removed. Your individual operation will determine your management, those requiring more extensive surgery may need a longer hospital stay, however, in most cases, the day following surgery your drip will be removed and your wound will be checked. You will be encouraged to get out of bed and move around the ward. If you have any problems the physiotherapist will see you to explain correct posture and the exercises that you will need to do. A copy of these exercises is enclosed in this booklet. You will need to bring this booklet into hospital with you so that you can start your exercises the day after your surgery.
The physiotherapy section gives you advice on what you should be doing when you go home.
Taking the wound drain out requires the nurse to remove the stitch holding it in place and gradually slide the drain tube out. It is not normally painful and they are usually easily removed. In very rare circumstances the drain may need to be removed in theatre however this exceptionally rare.
If you have not already been out of bed you will be expected to get out of bed and move around. You may be seen by a physiotherapist if needed, however a copy of the exercises are in the back of the book to aid your recovery. You will need to bring this booklet into hospital with you so that you will know what your exercises are and so that the Physiotherapist can complete the individual details for your exercise programme whilst explaining it to you.
Some patients will require an x-ray of their surgical level the day after surgery, this depends on the type of surgery performed. The medical staff will make this decision based on each individual patient.
One of the medical/specialist nursing team will check how you are managing. Following this you will normally be able to go home late morning or in the afternoon. It is quite normal practice to go home the day after your operation for most operations. Occasionally some patients who have had more extensive surgery may need some extra time in Hospital to recover. This is often just an extra day and is not usually more than a few extra days.
Pain medications
You may be taking two types of medications for pain, many patients come in for surgery having taken pain medication for a long time, such as Gabapentin, pregabalin, Amitriptyline, Duloxetine etc. Your doctor or specialist nurse may recommend, following your surgery, that you take a strong opioid medication alongside other painkillers such paracetamol and your usual medication. This is to relieve the additional pain that your injuries, illness or surgery has caused.
When you are discharged, as well as your normal medication, you may be given strong opioid medication to take home. It is important that you do not exceed the maximum dose prescribed for you. It is also important that you do not take any other painkillers that have not been prescribed by the hospital at the time of your discharge. This may result in you having too much pain medicine and cause the risk of severe side effects.
If you were not already taking opioid medicines before admission to hospital, you should not need to take them for a long time. The additional pain medication, prescribed whilst you are in hospital, is only intended to be short term. As you recover and your pain reduces you will be able to slowly reduce taking the medicines.
Any medication you were taking prior to surgery should not be stopped suddenly and once you have recovered from surgery, after a few weeks, as your pain settles discuss with your GP about a reducing regime for your medication You should ask your GP to review your medicines to ensure you are not taking them longer than necessary and also to ensure they are reduced safely as abruptly stopping of some medications can produce side effects.
Discharge home
Getting home
Please arrange for a relative or friend to collect you. You will not be able to drive or use public transport. You can go home by taxi if a member of your family or friend can accompany you. If you are travelling in a car, sit in the passenger seat and recline this to make it more comfortable for your journey home. If you cannot get transport arranged then we can arrange hospital transport, however travelling with a relative or friend would preferable if you can organise this.
Medication
Medication can be organised for you to take home, if required. Unfortunately, if we arrange medication from our pharmacy then this can mean you need to wait until later on your discharge day for it to arrive.
Sutures
Some patients will have dissolvable stitches in place, some will have stitches that need removal, and some may have metal clips. Your stitches/clips will be due to be removed approximately 7-10 days after your surgery (in some cases longer, but this will be clarified with you before you go home). Most patients make an appointment to get this done by their GP or Practice Nurse. If you do not have access to this then a District Nurse can be organised to check your wound and remove your stitches (dissolvable stitches will only need to be trimmed at the ends). If needed then the date of your District Nurse visit will be given to you before you leave the ward. Please make sure that if you are not going home to your usual address and you are going to stay with someone else you inform the staff to ensure that the District Nurse comes to the correct address.
Wound care
Should you have any problems with your wound after your surgery, even if your GP or District Nurse are managing this, it is very important that we are also informed as we may need to monitor you more closely. We would like you to contact us if there is any redness round the wound, wound leakage, or you have a temperature.
Please phone either:
- Spinal Nurses on 0151 556 3424
- Tissue Viability Team on 0151 529 5599
You can shower, but please aim to keep the wound dressing dry, until it has healed and any sutures/clips have been removed.
Pain
It is not unusual for you to get increased pain or altered sensation for a few days to a few weeks after surgery as your spinal cord and/or nerves recover from your surgery. It is important that you stay mobile and continue with your physiotherapy exercises following discharge. Some patients will experience a flare up of symptoms/pain approx. 7 -10 days post-surgery, this usually settles over time, but it is not unusual to get fluctuations in pain/symptoms over many weeks/months.
Activity
Remember that you have had an operation and it is usual to feel tired after this. Pace yourself and gradually build up your level of activity. Doing small things often, rather than all in one go is more sensible. You should progressively return to your normal daily routine as quickly as possible. You can undertake all the usual activities of daily life as you feel comfortable. This includes walking, shopping, driving and sexual activity.
Research has shown that patients who return to normal routine as quickly as possible make the best recovery. You should progressively return to your normal daily routine as you continue to recover. You can return to work as soon as you feel you can cope even if you feel uncomfortable. Heavy lifting should only be performed in the correct way and should be avoided for the first three months.
Surgical stockings
You should wear your surgical stockings for up to six weeks post-surgery, if your mobility is restricted or two weeks if you are fully mobile to reduce the risk of DVT (blood clots in the legs), and we advise not to fly for six weeks post surgery, again due to the risk of DVT.
Driving
You can drive when you can have a full range of movement and you must have full movement to allow you to have full control of the car, this includes being able to do an emergency stop. This is usually a few weeks after surgery.
Work
You can return to work when you feel able and this can depend on what your job role involves. Those with desk based roles may feel comfortable to return to work four to six weeks post surgery, but would need to be able to get up and move around to prevent stiffening in the back area. Those with more manual jobs may need to wait the full three months before being able to return. Please discuss this with your nurse specialist or medical team if you are unsure.
When will we see you
You will be sent an outpatient appointment for approximately three months following surgery by post to either come and see us, or for us to speak to you by phone, so we can check you are recovering well. Here you will be seen/spoken to by either a doctor or a nurse specialist.
Concerns
If you have any queries before then please do not hesitate to contact the spinal nurses on the advice line 0151 556 3424. Please leave your name and telephone number clearly on the answer machine so we can call you back. We try to answer the messages every working day. We work Mon- Fri 8am-6pm, we do not work weekends. We do spend a lot of time on the wards and in the out-patient clinics seeing patients, so please be patient, we will call as soon as we can.
Physiotherapy following lumbar spine surgery
This information is intended to answer the most commonly asked questions. Any further enquiries can be directed to the Physiotherapy department.
On your first day post operatively, it is perfectly safe to:
• Be up and walking around.
• Perform daily activities such as dressing and washing.
• You may experience some hip and back discomfort; this is due to the position you were in (in theatre) and is normal. This will resolve in a few days.
• Spend time sitting out in your bedside chair, regularly changing your position is advised.
General advice
It is safe to continue with all regular activities such as cooking, cleaning, shopping and sexual activity.
You can sleep in whatever position is easiest for you.
You may continue to have some back/leg discomfort or changes in sensation especially for the first 12 weeks, this is normal.
There is no evidence to say that returning to activity and exercise leads to any adverse effects or the need for re-operation.
Symptoms to report
These are rare however if you develop any of the following symptoms you should seek medical advice without delay:
• Difficulty passing or controlling urine
• Numbness around your back passage or genitals
• Numbness, pins and needles or weakness in both legs
• Unsteadiness on your feet
Lifting
There is no restriction in bending forwards to pick up light objects or putting on your shoes and socks. We think it is sensible to avoid heavy lifting where possible to begin with. You can resume lifting when you feel able to do so. There is no given weight we advise as everyone has their own usual capabilities. You can gradually increase the amount you do until you are back to your typical ability.
Driving
You can return to driving as soon as you can sit comfortably, perform an emergency stop and that you feel safe to do so. This is a self-certification.
Work
Returning to work and normal activities will help your recovery and you should aim to do this as soon as possible. People who return to work sooner have been shown to have better outcomes. You can return to work as soon as you feel you can cope, even if your back is still uncomfortable. You may wish to grade your return to work. It may take slightly longer to be able to return to a more ‘manually heavy’ job, this can be discussed with the relevant staff members. It is normal to feel tired when returning to work after a period of sickness absence. You should plan to pace yourself and take regular breaks.
Exercise
General activity and exercise has been shown to be safe in this patient group and indeed is beneficial for your overall health. We have included an exercise programme however general activities that you may already enjoy have been proven to be as effective therefore you should look to gradually resume these. For example, hiking, swimming, cycling, jogging, yoga and pilates. Keeping a record/ diary may help you in guiding your progression. Some discomfort is normal when restarting activity; you should work within reasonable limits. Lower intensity exercise should be started first progressing to higher intensity over a period of weeks.
You can also safely return to recreational sports such as football or golf in a gradual manner. For specific advice with regards to contact sports/ extremes of exercise this should be discussed with your medical team.
Physiotherapy following surgery
This information has been designed for post-operative back care. It is intended to answer the most commonly asked questions. Any further enquiries should be directed to your physiotherapist. You may see the physiotherapist the day after your operation, or you may attend a physiotherapy group the day before or after your surgery.
Exercise programme
Exercises to be completed in sets of 10, 1 - 2 times each day. These exercises can be complemented by activities such as swimming, yoga, pilates and any other activity which you normally enjoy
START POSITION: Lying on your back with both legs bent and your knees together.
ACTION: Slowly roll your knees from side to side keeping your upper trunk still.
START POSITION: Lying on your back with knees bent feet on firm surface (bed/floor).
ACTION: Pull pelvic floor muscles in and lift your bottom off the bed. Hold for 10 seconds then relax. Repeat exercise 10 times.
START POSITION: Lying on your back.
ACTION: Bend the leg to be stretched forward towards your chest and hold with both arms. Hug both knees to chest. You should feel the stretching on the back of your thighs and buttock. Hold 10 seconds, repeat 10 times.

START POSITION: Lie on the back with both legs straight. Bend one hip to 90 degrees and hold the thigh.
ACTION: Hold 10 seconds then relax. Repeat 10 times. Holding the thigh in position, slowly straighten the knee until a stretch is felt at the back of the thigh. Hold 10 seconds then relax. Repeat 10 times.

START POSITION: On hands and knees with the knees under the hips and the back relaxed in a neutral position. (Feet relaxed).
ACTION: Suck in your tummy muscles and keeping the back flat slowly rock backwards moving at the hips. Do not let the back bend or arch. Move back towards the heels until you feel the pelvis start to give. ONLY move backwards as far as the controlled flat back allows. Move slowly and do not stretch. This exercise may not be suitable for people with existing hip or knee problems.

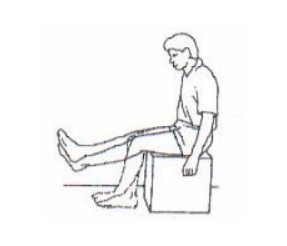
START POSITION: Sit upright with your legs side by side.
ACTION: Alternately straighten your legs and then bend each leg allowing them to swing. Do not do so much as to make it painful.
START POSITION
Sit on a chair with your legs apart.
ACTION
Bend your head down and trunk down between your knees rounding your upper body as far as feels comfortable, bend forwards, you may experience some back stiffness. Return to upright sitting. Repeat 10 times.

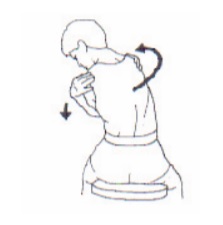
START POSITION
Sit on a chair and cross your arms over your chest clasping the opposite shoulder.
ACTION
Bend your upper trunk forward while at the same time rotating and side bending to the same side. Let your eyes follow the movement. Breathe out during the exercise.
Preventing recurrences
- It’s your back! Maintain your good posture in sitting and standing.
- It’s your back! Immobility leads to pain, to more immobility, to more pain; hurt does not mean harm, so continue with your exercises.
- Live life as normally as possible, keep up daily activities, and try to stay fit.
- Be patient. It is normal to get aches or twinges for a time.
The information contained in this booklet is a guide to help you understand what to expect. It may be that in order to address individual needs your experience is slightly different from that described.
If you have any queries, before or after, your surgery please feel free to contact us:
- Spinal Nurses 0151 529 8853
- Physiotherapy team 0151 529 5451
- Secretary to your consultant via hospital switchboard on 0151 525 3611
If you require this information in other formats or languages, please speak to a member of staff for details.
The references used in compiling this information are available on The Walton Centre website or on request.
Glossary of terms
MRI scan
This is a scan that uses the magnetic fields of the cells in the body. It can provide very detailed images of both head and spinal structures. It requires the person having the scan to lie still in the scan tube for approximately 30mins. Any movement can distort the final images so it is very important to remain completely still for this type of scan.
CT scan
This type of scan is useful for giving accurate pictures of the structures within the spine, especially detail of the bony structure. It uses x rays in a particular way to form the pictures.
Spondylosis
Degenerative changes in the joints of the spinal column, usually as a result of osteoarthritis.
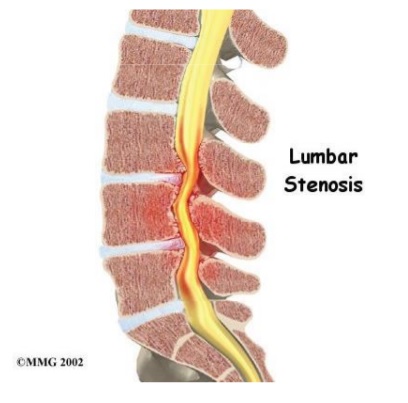
Stenosis
Spinal stenosis is when the spinal canal is too narrow and the spinal cord/nerves become too tight in the narrowed space. This can be due to congenital narrowing or degenerative changes. A laminectomy (see next page) is often performed to give the spinal cord/nerves more space.
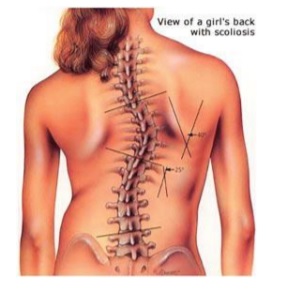
Scoliosis
Abnormal curvature of the spine.
Spondylolisthesis
This is a forward slip of one of the bones of the spinal column on another. This can occur due to degenerative changes or trauma. It can cause narrowing of the canal in which the spinal cord / nerves run and as a result can put pressure on the spinal cord or nerves.

Radiculopathy
This is the name given to problems, for example pain or weakness, that occur as a result of pressure on a particular individual spinal nerve root (rather than multiple different nerve roots).
Cyst
A fluid filled cavity
Syringomyelia
This is the development of a fluid filled cavity within the spinal cord. This can be associated with other conditions or the result of trauma. The spinal cord around the cavity can become compressed as the cavity expands.
Osteophyte
This is a bone spur. These bones projections form along joints and occur naturally in the spine as a person ages. They often only cause a problem if they cause any pressure on the spinal cord and/or nerves.

Surgical procedures
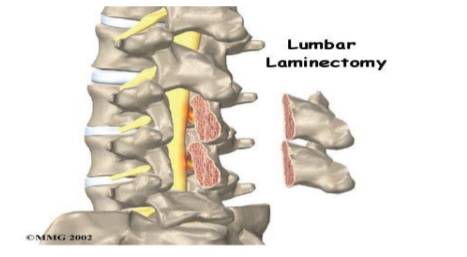
Laminectomy
This is a surgical procedure to remove the lamina and spinous process. Both of these are parts of the bone that encircles the spinal cord/nerves and they are at the back of the bony spinal column. This is done in order to provide access to the spinal cord and nerves for surgery or to release pressure on the spinal cord and/or nerves.

Decompression
This is when the cause of any pressure to the spinal cord and/or nerve roots is surgically removed. They are decompressed.
Facetectomy
This is the name given to the surgical procedure to remove part of the facet joint of the vertebral column. The facet joints are on each side of the vertebrae just by where the nerve root comes out from the spine. Sometimes these joints can become too big (especially as we get older) and cause pressure on the nerves lying next to them.
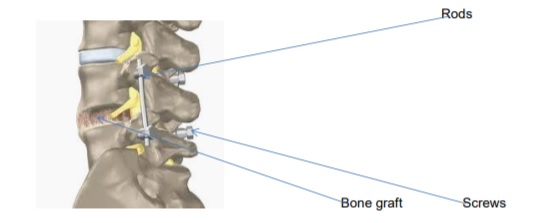
Fusion
This is an operation to join two or more vertebrae of the spine together. This is often performed to stop/reduce abnormal movement of the bones (vertebra) that can cause pain, or problems with the function of the nerves. It sometimes needs to be performed to stabilise any bones that have become unstable as an unavoidable result of a surgical procedure. The bones are fused together using your own bone, donor bone with or without metallic screws, rods and plates.
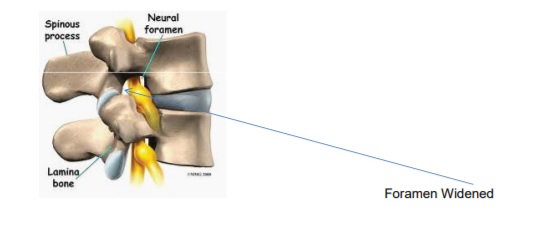
Foraminotomy
This is a surgical procedure when overlying bone is drilled away from the nerves that are underneath to release any pressure from the bone on those nerve roots.
Vertebraplasty
Injection of a form of cement into a particular bone or bones of the spinal column to make them more stable.

Kyphoplasty
This is the same as vertebraplasty with the addition that the bones of the spinal column, at the particular level are manoeuvred into a better position by a small balloon, before the cement is injected.
- Last Updated:01 February 2024
- Review Date:29 February 2028
- Author:Spinal nurses
- Summary:
Information to help you understand what will happen to you during your time with us for lumber spinal surgery. It also contains your physiotherapy exercises for you to do following your surgery and some general advice following lumbar spinal surgery.