Spinal fractures (Traumatic)
This information leaflet has been designed to inform you about your spinal fracture. It will explain: how your fracture will be managed, how you can support your recovery and also answer some common questions. It is a general guide therefore individual advice may vary for each person.
What has happened to me?
You have broken (fractured) one or more of the bones (vertebrae) in your back (spine).
Why has this happened to me?
This may have been caused by a traumatic injury causing excessive force to your back.
What does my back look like?
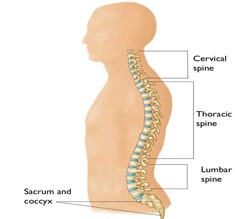
Your back runs from the bottom of your skull to your pelvis. It is made up of bones that are all stacked up on top of each other and supported by ligaments, with soft cushions of discs (intervertebral discs) in between each of the bones that act as shock absorbers. The bones each form a circle (spinal canal), which the spinal cord and nerves pass through. The bones provide protection for the spinal cord and nerves which are important as they pass information from the brain to your body about movement, pain, touch (sensation) and other important body functions.
What will happen with my spinal fracture?
Breaks (fractures) in the spine can be stable or unstable.
Stable means that the majority of the spinal structure is still intact so it is unlikely to move. These fractures are usually managed conservatively. Conservatively means there is no need for an operation. You may be managed in an orthosis, such as a collar, halo jacket or brace, or may need nothing doing at all. You may receive an additional leaflet with more information if you are treated with one of these orthoses.
Unstable means the spinal structure has been affected, and could have moved or is at risk of moving which may cause further complications. An operation may be offered for this type of fracture in order to provide support to the spinal structures. Metal work (Instrumentation) in the form of screws, rods and plates are usually inserted to act as scaffolding to support the bones whilst they heal. These are usually left in place and not removed even after the fracture has healed.
What should I expect after my fracture?
Whilst the doctors are assessing how best to manage your fracture, or whilst you are waiting investigations such as x-rays or scans, you may be asked to stay flat in bed (bed rest). This could result in joint stiffness or weakness. You may be provided with bed exercises to complete whilst on bed rest. Once the doctors have decided on a plan of how to manage your fracture you will be allowed to get up, move about and sit out in a chair. Support will be offered, if required, to ensure you are safe. It is not unusual to have feelings of light headedness or dizziness and also pain the first time you get up. You may also experience some of these symptoms after surgery but they are normal symptoms to expect after a period of not moving or after a surgical procedure.
When you sustained your injury there may have been some damage to the spinal cord or nerves due to the fracture, force of injury, or even swelling or bruising. This may cause you some problems with movement, sensation or other body functions. You will be assessed by a physiotherapist, and if needed other members of the specialist team, such as an occupational therapist, to support your recovery and rehabilitation.
How does a fracture heal?
Fracture healing is a complex process and can be influenced by a number of factors such as how your injury occurred, your general medical condition or any other health conditions. Some reasons to take into consideration include age, nicotine intake, long term steroids use, poor diet and also conditions such as Osteoporosis, Diabetes, Hypothyroidism, excessive chronic alcohol use.
When will my fracture heal?
A fracture can heal by either bone fusion or by fibrous union. Generally we give a period of 12 weeks to allow this process to occur. However, in a very small number of spinal fractures they do not heal at all, even when they get the best surgical or conservative treatment. In some cases, certain risk factors make it more likely that a bone may not heal. You may hear the term ‘non-union’ this is when a broken bone fails to heal. The term ‘delayed union’ is when a fracture takes longer than usual to heal. Fibrous union means the fracture is filled with strong enough scar tissue (but not bone cells) to prevent movement at the fracture site, which makes the fracture stable enough to wean from any brace and get back to activities.
Will I have any pain and how will it be managed?
Fractures are painful and pain can still be present as you continue to recover and your bones heal. The healing process often takes 3 months, but the majority of pain settles by week 6. Regular pain killers may be needed. Paracetamol and Ibruprofen (if tolerated) are effective and can be purchased over the counter. You may require pain killers in hospital. A 14 day supply of medications will be supplied on discharge, if required. A discharge summary is sent out to your GP and any further supply will be arranged by your own GP practice. Some pain killers can cause constipation. A healthy, well balanced diet can help reduce this. For more information visit: www.nhs.uk/conditions/constipation/
What can I do to support my recovery?
Continue to walk if it is safe for you to do so and gradually increase the distance and number of times that you walk each day.
Continue to complete your day to day activities such as dressing, washing, cooking but try to avoid any tasks that require repeated and heavy lifting initially.
Good posture is important as it minimises strain on the spine. It is important to try to maintain the normal curves of the spine .You should particularly try to avoid: (i) head forward and slouched shoulders, (ii) slumped sitting positions. You should also try to maintain a good posture and correct technique when lifting (remember to avoid lifting anything heavy initially), such as bending the knees, keeping good posture, standing up by straightening the hips and knees, avoiding twisting or rotating. The physiotherapist may go over posture and lifting with you in more detail and can provide specific exercises.
If you have been asked to wear an orthosis by your team, such as collar, halo jacket or brace please refer to your separate leaflet for that orthosis which will explain more regarding bathing or showering. If you have a surgical wound you should avoid getting this wet for a minimum of 7 days after surgery.
You can sleep in whatever position is easiest for you; however some orthoses may limit your comfort in certain positions.
You should aim to return to work as soon as you are able to, however the timescale for returning to work will vary depending on your occupation. Please discuss this with your specialist team. We would advise a staggered or graded return to work. Your own GP or work occupational health department may be able to support you with this.
If you are in college or university it is likely that you will be able to continue with your studies as soon as you feel able to. However we advise you contact your personal tutor for more advice and to discuss your individual requirements and those of your course.
Additional physical activities including low impact exercise such as static bike cycling or pilates may be possible to build up to after discharge but discuss these with your specialist team. If you have been asked to wear a collar or spinal brace your specialist team may want you to avoid even low impact exercise until you have been reviewed in clinic and the collar or brace has been removed. Higher impact activities such as running, weights and impact sports should be avoided until discussed with your specialist team at your follow up appointments.
You may have been provided with a specific exercise programme which you should continue to complete according to the advice given by the physiotherapist.
You will be given advice regarding driving. If you are in a collar, halo jacket or spinal brace the DVLA do give strict guidance. Otherwise you will need the range of movement to see safely and also perform an emergency stop.
In order to support your body to heal; you should eat a balanced healthy diet and avoid alcohol and smoking.
What should I expect after being discharged?
Mild to moderate pain is to be expected because of the injury you have sustained and any surgery that has been performed. If you have difficulty managing your level of pain, which is not relieved by your pain killers, then you should speak to your spinal nurse specialist or attend your GP practice or Pharmacy
It is normal to experience altered sensations including pins and needles and muscle spasms after a fracture. Nerve recovery can be slow and take many months. It can be up to 24 months.
If you have any change in the power to your arms or legs, reduction in the sensation to your arms and legs, numbness in the genital area or problems with your bladder, bowel (particularly incontinence) or erectile function or experience new severe pain you should attend your local A+E department. Your local A+E can liaise with your spinal team.
If you notice any problems with your surgical wound site such as excessive redness, warmth or leakage, particularly if you also have a raised temperature, you should contact your nurse specialist or call the ward you were discharged from, attend your GP practice or local hospital.
If you fall and injure yourself you should call your spinal nurse specialist team or attend your local A+E department.
Your specialist team will advise whether you should attend clinic. Often this can be on a regular basis, for fractures managed conservatively, for investigations such as x-rays at 2, 6 and 12 weeks. If your fracture has been managed surgically then you may attend at 3 month, 1 year and then subsequent yearly intervals. It is important that you attend the outpatient appointment if offered, even if you may already be undergoing check ups with another consultant.
Your first follow up appointment has been made for:
……………………………………………………….
Additional advice specific to you:
Who can I contact after I have been discharged if I need any advice?
- For help from a GP – use your GP surgery's website, use an online service or app, or call the surgery.
- For urgent medical help – use the NHS 111 online service, or call 111 if you're unable to get help online.
- For life-threatening emergencies – call 999 for an ambulance
- Walton Centre Spinal Trauma Clinical Nurse Specialist: 0151 556 3242.
- Walton Centre Acute and Trauma Physiotherapist team: 0151 556 3863
Your notes:
- Last Updated:01 March 2023
- Review Date:01 March 2025
- Author:Faye Mangan
- Summary:
This information leaflet has been designed to inform you about your spinal fracture. It will explain: how your fracture will be managed, how you can support your recovery and also answer some common questions. It is a general guide therefore individual advice may vary for each person.