Subarachnoid haemorrhage no cause found
What is a subarachnoid haemorrhage (SAH)?
A subarachnoid haemorrhage is bleeding in the space that surrounds the brain below the arachnoid membrane covering the brain. (See picture below)
Subarachnoid Haemorrhage occurs suddenly and usually without warning.
Symptoms are a sudden, severe headache and often accompanied by sickness, vomiting, neck stiffness, photophobia (dislike of light). In some instances, there is also loss of consciousness and/ or a seizure (fit). There may be difficulty with speech, disturbance in vision or a weakness in an arm or leg.
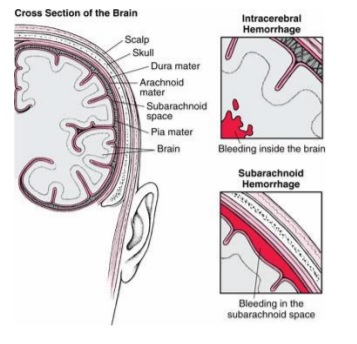
There are 3 membranes
covering the brain known as the meninges;
(The pia, arachnoid and dura)
The blood vessels within the brain lie below the
arachnoid membrane.
Could it have been prevented?
NO!
Diagnosing a subarachnoid haemorrhage
Diagnosing a subarachnoid haemorrhage is done initially from your history. It is confirmed by a head scan and occasionally a lumbar puncture.
If the tests appear positive, you will be transferred to the Walton Centre for further investigation.
You will undergo bed rest and be closely observed in the ward environment.
You will be given regular pain relief and medication to help prevent sickness/vomiting. Laxatives will also be offered as pain killers can cause constipation.
You are usually required to drink plenty for about 2 weeks if you are able. This is either by drinking or by a “drip” (intravenous infusion) into the vein. Plenty of fluids help keep a good blood flow to the brain. You may be required to take up to a 21-day course of tablets called Nimodipine. These have to be taken every 4 hours and help prevent complications due to the haemorrhage. If no cause is found, nimodipine may be discontinued but this would depend on the results of the initial scan.
Investigations to find a cause
You will undergo a brain scan with injection with contrast which shows the blood vessels within the brain.
CT angiogram: This is called a CTA (Computerised Tomography Angiogram). If no cause can be found then after the doctors review your case you may require a more formal angiogram –DSA (Digital Subtraction Angiogram). This is repeated in many cases after you have been given time for the blood in the brain to settle and reabsorb.
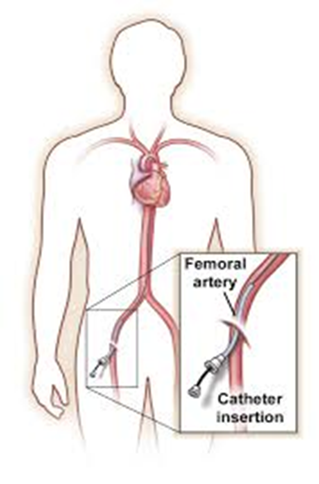
Digital Subtraction (formal) Angiogram: This is a test which involves the injection of dye through a catheter (tube) inserted into an artery in the groin which is then passed up to the brain through major blood vessels and a series of x-ray pictures are taken. This shows clear pictures of the blood vessels within the brain. You may be given provisional results immediately, but formal results are given once these pictures are reviewed in depth by your medical team. There is a separate information leaflet regarding the angiogram which you can request when you sign consent
Angiogram
No vascular abnormality found
In many cases a cause is found such as an aneurysm (or blister) on the blood vessel and this is then treated.
In approximately 15% -20% of people who are admitted to the Walton centre after a subarachnoid haemorrhage, no vascular abnormality is identified.
It is not always known exactly why such haemorrhages occur, but it is known that the risk of a future haemorrhage is extremely low and the outlook for recovery is positive.
When no cause is found, no treatment will be required other than to support you through your illness and manage your symptoms.
Your case and the tests we have completed will always be discussed at our multidisciplinary team (MDT) meeting for your safety and reassurance. You will be updated of any management plan as a result of that meeting.
Whether a cause is found or not you will still need to recover from the Subarachnoid Haemorrhage itself.
Some people are well soon after their subarachnoid haemorrhage, but many can be really poorly and need some time to stabilise and recover. Some people may need a period of rehabilitation before they are able to go home.
Everybody is different and your well being and recovery is usually dependent on how much blood there was in your brain, where it is and how the blood on the brain affects you.
Hydrocephalus
Rarely people can be unwell and need care on the intensive care ward after a subarachnoid haemorrhage despite the fact no cause is found. The most common reason for this is hydrocephalus.
Hydrocephalus is a condition where there is a build-up of cerebrospinal fluid (CSF) in and around the brain and spinal cord. This happens because it may not be able to drain away after the haemorrhage. Hydrocephalus can occur acutely after the initial bleed or whilst you are in hospital or less often, slowly after you have gone home.
Treatment for hydrocephalus includes an external ventricular drain (EVD) which may need to be inserted urgently whilst you are in hospital or a Lumber drain in the spinal cord.
If it becomes evident you need more permanent draining of the CSF you will need a shunt which is a more permanent drainage tube that allows the fluid in the brain to be drained into the sterile cavity in your abdomen.
Symptoms include a build-up of headaches, increasing drowsiness, problems with balance, possible problems with passing urine (incontinence) and possibly worsening vision and memory/concentration (more obvious than when you left hospital) These symptoms must not be ignored. If they are getting worse, you must go to your nearest accident and emergency department for a scan or let us know. Hydrocephalus can be treated by a shunt.
If you have a shunt, you should have information on it.
Support and information on shunts is available.
You cannot drive for 6 months if you have had a drain or shunt inserted.
Further Investigations:
In certain cases, further tests are necessary. These are specific to each individual case. They may include further blood tests whilst you are still in hospital.
It may be decided you need a delayed angiogram or an MR scan of your brain as an inpatient or after you go home.
You may require review and your care to be taken over by other doctors who are specialist in cases where no cause such as an aneurysm is found (vascular neurologists).
Going home:
Once it is decided that no further investigations are needed as an inpatient and your medical team are happy that you are recovering you will be allowed home.
You may need further investigations as an outpatient. The tests you will need should be discussed with you before you go home.
It is advised that you get your blood pressure and cholesterol checked by your GP about a month or so after going home.
Medication:
Nimodipine: You will normally stop this but some may be required to complete the 21 day course of Nimodipine. It is used to reduce the risk of developing complications with vasospasm (a process where the blood vessels close after a brain haemorrhage as a reaction to the blood). This risk has passed by 21 days and so the course doesn’t have to be continued. The tablets need to be taken regularly every 4 hours- if you miss a dose for more than an hour then it is safer to skip that dose rather than take two close together.
Side effects of Nimodipine are low blood pressure, flushing, changes in heart rate, headache, feeling sick and feeling too warm. Alcohol and grapefruit juice shouldn’t be taken along with Nimodipine as these may make side effects worse. Please read the leaflets accompanying the medicines given to you to take home from hospital.
Pain Relief: You may go home with pain killers. You should take these regularly to begin with if you need them. They should be cut down as soon as tolerated as taking them for too long may make headaches worse not better! That does not mean that you shouldn’t take them when needed.
Certain types of pain killers can cause constipation and so laxatives are usually given to you. Eating a diet that is high in natural fruit and fibre helps too.
If medication side effects occur, seek medical advice.
Extreme tiredness:
You will probably need rest once you get home particularly if you are having a lot of visitors or your house is very busy. Even simple tasks such as a walk to the local shop may leave you feeling exhausted. This will improve with time but may not go completely. You will know if you have done too much as you will be exhausted and may experience headaches. This often happens early evening or the next day and means you must rest! You should aim to have a rest each afternoon when you go home. Keep this for as long as you are benefitting from it.
Memory:
Some people may be left with poorer memory following a brain haemorrhage. Your memories before the haemorrhage will be less likely to be affected. This may improve with time but recovery can be frustrating as often your memory and concentration aren’t always as good as before. Try breaking down tasks into smaller steps and using a notice board or notebook to help you. Keeping your home organised and making lists helps A leaflet is available for helping with memory loss if this affects you.
Headaches:
Headaches are common after a subarachnoid haemorrhage. They usually ease with time. They may, however, persist. Headaches can be triggered by dehydration, stress, illness, too much or too little sleep and missing meals. Prolonged or regular use of analgesia (paracetamol, ibuprofen, codeine, morphine etc.) may also worsen or prolong headaches so should be used sparingly and stopped if no longer required. Drinking 2 to 3 litres of water per day, regular meals, ensuring a good sleep pattern and in some instances avoidance of certain triggers (caffeine, alcohol, cheese etc.) can help reduce the frequency and severity of headaches. There are also some treatment options such as menthol sticks to rub on the forehead which may help. Drinking more water and using pain relief at the start of a headache may also help.
Headaches are often worse if you have done too much that day or the day before.
If they persist despite you doing the above measures, then you may need help from your G.P. or a headache specialist
Pacing
You may benefit from pacing your activity for the first 4-6 weeks following going home. Take some gentle exercise. Build up activity as you feel able to and try to go outside for regular walks if you are able; otherwise you may lose your confidence and fitness. Aim to build up to half hour walks 5 days a week. You will probably need to take a rest each afternoon in the first few weeks of recovery.
Back Pain and other symptoms:
At the time of a subarachnoid haemorrhage, blood escapes from the artery into the fluid compartment of the brain called cerebrospinal fluid (CSF). This fluid travels around the brain and down the spinal cord in the subarachnoid space.
The blood should not be there and so it irritates the brain causing headaches as well as light hurting your eyes, sickness and sore neck.
In addition, when the blood travels down the spinal cord (usually when you start walking around) it can irritate the base of your spine and cause pain. Sometimes this can be severe and require regular or new medication to help. The pain usually settles down after a few weeks. If it does not, you should let your GP know.
Unusual sensations:
Some people experience unusual or strange sensations in their head following a brain haemorrhage. These are common symptoms and we are not sure why they occur. Do not worry about them as they usually ease with time.
Sensitivity to noise:
This is not uncommon following a brain haemorrhage. Everyday noise such as television or background conversations can be just as difficult to cope with as loud noises. This usually settles down with time as you recover.
Changes to smell and taste:
You may lose your sense of smell (and taste) after a brain haemorrhage. This usually (although not always) improves with time.
Epilepsy or “fits”:
Rarely people who have had a subarachnoid haemorrhage develop epilepsy causing “fits” or “seizures”. The risk is small for people whose haemorrhage we don’t find a cause for but at its greatest in the first 6 -12 months after subarachnoid haemorrhage. One fit does not mean you have epilepsy. If you have a seizure, you and your family will be taught safety advice and you may have to take anti-epileptic medication. This should never be stopped abruptly (unless it is only prescribed for a short time such as 2 weeks). Advice for safety with seizures is available via Epilepsy action https://www.epilepsy.org.uk/
Epilepsy is treated with medication. You will normally be reviewed by a neurologist to ensure appropriate management.
If you have had seizures, you have to inform the DVLA and cannot drive until advised. We can speak to you about this before you go home.
Fear of re-bleed:
This is a very common fear for all patients, particularly if no cause is found. The chance of another bleed is extremely rare and is usually no higher than everyone else in the general population.
Because your case has been discussed by the experts and we know the likelihood of another brain haemorrhage in these cases is extremely low, It is important to learn a coping strategy as this fear may prevent your recovery progressing.
In the unlikely event that you get the same symptoms as you did when you had a brain haemorrhage you need to go to your local accident and emergency department.
Recovery:
Recovery is dependent on how you feel.
You will need to pace yourself for the first month or more after going home because of tiredness and headaches. Save your energy for the things you have to do and those you want to do.
Looking after yourself in the early days of recovery is beneficial to your wellbeing in the long term.
Feelings of anger, frustration and sadness are not uncommon following a brain haemorrhage. This may be due to the condition but could just as well be due to the sudden life changing event and usually passes with time and support. If you are affected, you should talk to your GP as you may benefit from being referred for talk therapy or a psychologist to help you through this stage of recovery.
Family and friends
It is advised to have someone stay with you for the first week or so after going home.
Enlist the support of your family and friends whilst you recover. They will be a great help with shopping, transport and support and will be able to support you in your recovery. Making time for them will be beneficial in your recovery. If you aren’t feeling so confident just make plans for short visits or regular texts so that you don’t lose touch
Where can I meet other people who are going through similar experiences?
The “Brain Haemorrhage Support group” affiliated to the Walton Centre offer emotional support and practical (not medical) advice from personal experience (details in the back). Support is also available from the brain Charity in Liverpool, BASIC in Manchester and you can self-refer to local counselling services
There are details of the brain haemorrhage support group, and other links you may find useful in contact details at the back of this booklet.
Everyday Activities
Driving:
DVLA guidance changes all the time and so please check the advice available on the direct. gov website
Following a subarachnoid haemorrhage, if you hold a driving licence, you are legally required to notify the Driver and Vehicle Licensing Agency (DVLA). In your case they will need you to confirm that you have had a confirmed subarachnoid haemorrhage and no cause was found after a “comprehensive angiogram”.
The DVLA states you cannot drive following brain haemorrhage where no cause is found until you have recovered and received the go ahead from them: This is because driving involves many different cognitive and physical skills as well as multi-tasking, decision making and problem solving.
You cannot drive if you have new visual problems, cognitive problems or stroke like symptoms
You cannot drive if you have had a seizure (or fit) as a result of the subarachnoid haemorrhage.
DVLA guidance for management of subarachnoid haemorrhage is updated a number of times a year and so you can get up to date information from their website.
It is easier for you if you download and print off form B1 to send to The DVLA rather than wait for them to post it to you
Returning to work:
You can return to work as soon as you feel able from about 6 weeks following your brain haemorrhage. It will not make you ill to return sooner if you recover sooner and want to or must for financial reasons.
Most people, however, need about 3 months to recover. (Occasionally longer if there have been significant problems)
You will benefit from going back to work on a phased return. This means you build up your working days and hours according to how you are feeling. A phased return is often graduated over 4 weeks or longer and your employer has an obligation to adhere to it.
Brain Charity will help you if you are having problems with returning to work. The number is printed at the back of the booklet.
Access to Work- https://www.gov.uk/access-to-work gives advise and the Brain Charity - https://www.thebraincharity.org.uk can support you when you go back to work
Will I be entitled to any benefits?
You may be entitled to sick pay from your employer, or you are likely to be able to claim benefits appropriate to your specific situation. You should contact a charitable agency such as Citizens Advice Bureau, Welfare Rights or Brain Charity to discuss individual circumstances and what you are entitled to. Access to work accessible through https://www.gov.uk/access-to-work
Drinking Alcohol:
Do not drink alcohol until the 21-day course of nimodipine is completed and you have reduced the number of pain killers you take. However, most people find they are not able to tolerate large amounts of alcohol and their recovery benefits from reducing intake in the early stages
Details of an information website on alcohol awareness is printed at the back of this booklet
Smoking Cigarettes:
It is advisable that you give up smoking completely. A free help line number is printed at the end of this booklet.
Sexual Activity:
You can resume sexual activity as soon as you feel able.
Starting a family:
You can start a family as soon as you have concluded investigation and have results that all is well.
You will benefit from taking a few months to recover your physical fitness before planning a family. You will not normally be prevented from a normal delivery but this will depend on your obstetrician.
Exercise:
Extreme exercise should be avoided until all delayed investigations are complete and results have been given.
Exercise is encouraged as it improves stamina and wellbeing. Most sports can be resumed once you feel able. You should build up your fitness slowly as soon as you feel able. It is advisable to go swimming with somebody during the first year following your brain haemorrhage.
Dental treatment:
Dental treatment is safe after SAH. Your dentist may need to seek advice from your consultant or GP if you are taking aspirin.
Flying:
If you have had a Subarachnoid Haemorrhage with no vascular abnormality found, you should be able to fly as soon as you feel able.
If you have more specific questions please ask your neurovascular nurse specialists, medical team or ward nurses.
Going home information
Name:
Consultant:
Date of Sub-Arachnoid Haemorrhage:
Follow up advice:
Activity:
- Build up activity as you are able:
- You will benefit from building up your activity slowly starting with a short walk and building up as you feel stronger
- You should pace activities and rest each day until you feel more recovered.
- You should have a rest each afternoon for the next few weeks in order to support your recovery
- You will benefit from keeping hydrated, a regular sleep pattern and regular meals.
- You may need a little more sleep than normal in the first week after going home but this will gradually improve
- Driving: According to DVLA guidelines – You must not drive and must notify the DVLA.
They need clinical confirmation of your recovery and confirmation that no cause has been found. - Working: At least 6 - 12 weeks. This depends on how you feel and most people need about 3 months. When you do go back to work you will need a phased return and undergo regular risk assessment of your well-being. Your employer may need to make adjustments to support your recovery.
- See your GP for blood pressure and cholesterol in a month unless otherwise specified.
- More specific recovery advice is in the information leaflet you have been given for subarachnoid haemorrhage “No cause found”
Medications:
Pain relief (aim to be off all regular pain relief in a month: if you can’t reduce pain killers for headache you should let the neurovascular nurses know as more specialist input may be required)
Appointments:
- Phone call to check on your wellbeing (usually between 4 and 6)
- Nurse clinic 2-3 months
- Delayed MRI/A brain scan
- If you need any advice then please call the nurse helpline on 0151 556 3325 (Your consultants secretary is responsible for your DVLA form though)
ADVICE FOR CARING FOR PUNCTURE SITE TO GROIN/WRIST POST OPERATIVELY.
If the problem is considered serious, help should be sought from your local accident and emergency department immediately. Otherwise, you should contact your G.P., NHS direct or visit your local walk in centre.
- Do not strain or lift anything greater than 10lb for 10 days following angiogram
- Drink plenty of water or juice 24 hours before and 24 hours after the angiogram to prepare the kidneys and flush the dye from your body (about 2 litres or 10 glasses)
- Do not drive or operate machinery for 24 hours following angiogram
- Do not do any physical exercise or sexual activity for 24 hours following the angiogram.
- Keep the dressing on, clean and dry for 24 hours following the angiogram
- After 24 hours the dressing can be removed and a shower (not bath) can be taken. A bath and swimming is allowed once the site is fully healed.
- Clean and inspect the site and wash with mild soap and water. Dry and re-cover with a plaster until it is healed completely
- Report to A+E if the site bleeds and not stopped after 15 minutes of firm (but not excessive) manual pressure.
- Report to your doctor/ us/ A+E depending on the severity if there is any swelling; change in colour (paler or darker); change in temperature or change in sensation to the leg/hand.
- Report to your doctor if there are any signs of infection such as redness, pain, swelling or pus from the site.
- Report to your doctor/ us/ A+E depending on severity if there are signs of excessive new bruising (a small amount of bruising is expected from the procedure).
- If you have a new lump in at the site of the angiogram puncture which pulsates you should cover it- do not mobilise and must have it seen to urgently: either go to A+E or inform us
- If you have had a puncture in the groin and develop pain in the abdomen (flank) on the side of the angiogram you must attend A+E or speak to us urgently
Self help
- Brain Haemorrhage Support Group offers practical advice and emotional support for all patients and their families/friends that have had a subarachnoid haemorrhage.
- Keeping a diary may help support your recovery and allow you to watch your progress.
- There are self-help leaflets available from your neurovascular specialist nurse if you are struggling with fatigue, poor memory, low mood, poor concentration or difficulty in decision making
- Your recovery will benefit from keeping active as you are able; staying hydrated, not missing meals and having a bed time routine.
- Brain Charity– Information and Support for people with neurological Conditions (Leaflet available at the helpdesk on the ground floor).
- BASIC in Manchester also offer help and support for people suffering from subarachnoid haemorrhage
- Information is available for all patients who have had shunts inserted as a result of brain haemorrhage. (Through your ward staff, neurovascular nurse specialist, hydrocephalus nurse specialist.)
- Information is available for all patients who have epilepsy as a result of brain haemorrhage. (Through your ward staff, neurovascular nurse specialist, epilepsy nurse specialist.)
- “Road to Recovery.” This is a voluntary information course organised and run by the neurovascular nurse specialists/Walton Centre and supported by the Brain Haemorrhage Support Group. It usually runs once or twice a year depending on resources and need. It is for those people and family / friends who have recently been affected by Subarachnoid Haemorrhage.
- Information about the course is available through your neurovascular nurse and customer care team. You can request an invitation to this course at any time if you think you may benefit.
Walton Centre Contact Details
For any emergency please attend your local
Accident and Emergency Department or see your G.P.
Patient Experience Team provides a PALS service. 0151 556 3091/3090/3093 wcft.patientexperienceteam@nhs.net
Neurovascular Nurse Specialists: 0151 556 3325 (Non-urgent enquiries as calls may not be answered the same day)
Walton Centre switchboard - 0151 525 3611
- Dott Ward - 0151 556 4276/3887
- Cairns Ward - 0151 556 3567/3568
- Caton Ward - 0151 556 3588/3894
- Caton Short stay ward – 0151 556 3576/3568
- Chavasse Ward - 0151 556 3897 / 3591
- Lipton Ward – 0151 556 3344/3383
- High dependency - 0151 529 5489
- Intensive Care - 0151 556 3462/3798
For information regarding appointments or DVLA please contact your
consultants secretary.
Useful Contact details
NHS 111: 111
Telephone advice if you need urgent medical help fast but it is not a 999 emergency (or you do not have a GP)
Website: http://www.nhs.uk and search ‘emergency and urgent care’
D.V.L.A. Driver Vehicle Licensing Authority,
Drivers Medical Group, DVLA, Swansea, SA99 1DL.
Medical Enquiries: 0300 790 6806
Downloading and printing form B1 may speed the process up for you
Brain Haemorrhage Support Group affiliated to Walton centre:
Facebook or via Brain Charity
The Brain Charity: 0151 298 2999. www.thebraincharity.org.uk
Advice regarding benefits or money problems after subarachnoid haemorrhage can be gained from the Brain Charity who have a stall in the outpatient department of the Walton Centre
Working Life Service at The Brain Charity: 0151 298 3288
BASIC Manchester: 0161 707 6441 https://www.basiccharity.org.uk/
Advice and support for people who live closer to Manchester
Epilepsy Action: https://www.epilepsy.org.uk/
Advice for people who have had seizures after a brain haemorrhage
Department of Work and Pensions: 0345 606 0265 https://www.gov.uk/government/organisations/department-for-work-pensions
Access to Work for support if you have a disability or health condition: https://www.gov.uk/access-to-work
NHS Quit smoking helpline:
England: 0300 123 1044 https://www.nhs.uk/better-health/quit-smoking/
Wales: 0800 085 2219 https://phw.nhs.wales/services-and-teams/healthy-working-wales/health-and-wellbeing-workplace-guidance/substance-misuse/help-me-quit
Advice on Alcohol: https://www.nhs.uk/live-well/alcohol-advice/alcohol-support
Drinkline: 0300 123 111
- Last Updated:01 April 2023
- Review Date:01 April 2026
- Author:C Stoneley
- Summary:
Diagnosis and treatment for a subarachnoid haemorrhage