Subarachnoid haemorrhage
Subarachnoid Haemorrhage
What is a Subarachnoid Haemorrhage (SAH)?
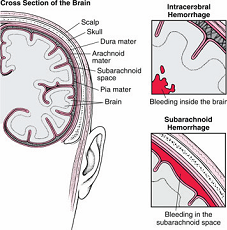
SAH is due to a leakage of blood from a blood vessel beneath the arachnoid membrane that covers the brain. (see picture below)
Sub-arachnoid Haemorrhage occurs suddenly and usually without warning. SAH causes a sudden, severe headache and is often accompanied by sickness, vomiting, neck stiffness, photophobia (dislike of light), sometimes with loss of consciousness and/ or seizure (fit). There may be difficulty with speech; problems with vision or a weakness in an arm or leg.
There are 3 membranes covering the brain called the meninges; the pia, arachnoid and dura. The blood vessels within the brain lie below the arachnoid membrane.
What Causes SAH?
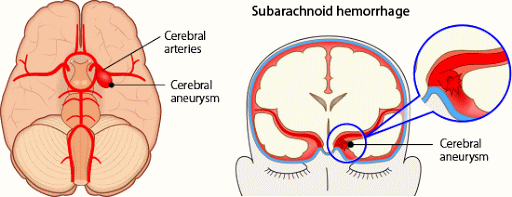
Aneurysms
- Aneurysms are the cause of 75% of subarachnoid haemorrhages. Aneurysms are a fault (or weakness) in a blood vessel wall. They are often berry shaped, like a blister.
- The ruptured aneurysm requires urgent treatment as once an aneurysm has bled there is a high risk of re-bleed in the short term.
- SAH from an aneurysm is most common in people between 40 and 60, although they can occur at any age.
Occasionally, more than one aneurysm is found. The aneurysm that has ruptured will be treated first. The unruptured aneurysms are not always treated at the same time. It is more usual to wait until you have recovered and come back later to have further aneurysms treated or they may be monitored. You will usually receive a plan regarding any unruptured aneurysms before you go home as discussions regarding management of these are normally made during your inpatient stay.
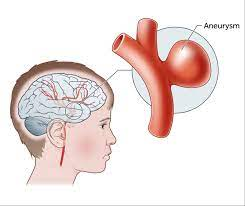
Diagram of a brain aneurysm
Could it have been prevented?
- NO!
There is no known reason why a haemorrhage happens at a particular time, but they can rupture at times of physical effort such as coughing, heavy lifting, straining or during sex.
Are there any warning signs?
- In most cases the aneurysm goes undetected until it bursts.
- Rarely an aneurysm can press on a particular part of the brain and cause symptoms.
No vascular Abnormality Found.
- In 15% of cases no vascular abnormality is identified. We do not always know why such haemorrhages occur, but we do know that generally the outlook is good and the risk of a future haemorrhage is very low.
- In cases where no cause is found, no treatment will be required. Although your recovery will generally ( although not always) be quicker, you will need time to recover from the bleed itself (a separate information booklet is available on this type of haemorrhage)
Is the Condition Hereditary?
Generally, aneurysms are not hereditary but appear to be due to family lifestyle such as smoking.
Routine testing of family members has been shown not to save lives, but family members can be referred for investigation for hereditary aneurysms once 2 first line relatives have been diagnosed with aneurysms. Referral is usually done by their GP to the local neurosurgical centre and will be considered on their individual risk First line relatives are your brothers, sisters, children, and parents.
They may also be considered for screening if there are a lot of people in your family who have had aneurysms or bleeds from aneurysms.
Finding an aneurysm that cannot be treated can be distressing and so it is important your relative is counselled by the specialist prior to agreeing.
First line relatives are: 1. your brothers and sisters and 2. Your children or parents.
To start this process, speak to your consultant neurosurgeon or specialist nurse. They will probably advise you to inform your relative to speak to their own G.P. and be referred to their local neurosurgical hospital.
Information on screening is available in a separate information booklet “Brain aneurysms and screening” or via NHS website ( details in “useful contact details” at end of this booklet).
Diagnosing a Subarachnoid Haemorrhage
This is usually made by the history of events leading up to, including and after the brain haemorrhage, CT scan and occasionally lumbar puncture.
If initial tests appear positive, you will be referred to the Walton Centre for further investigation and treatment if necessary.
You may then undergo a Computerised Tomography Angiogram (CTA) either in A+E or after you are admitted to the Walton Centre. This involves a scan after injection with contrast solution in the vein which allows the blood vessels within the brain to be seen clearly.
If an aneurysm ( or aneurysms) are found, treatment options will be discussed by your expert team which includes specialist neurosurgeons and specialist neuro interventional radiologists ( Consultant doctors who perform endovascular treatment via blood vessels
If no aneurysms are seen a Digital Subtraction Angiography (DSA) may be advised. This is a test which involves the injection of dye through a catheter (tube) inserted into an artery in the groin or wrist and a series of x-ray pictures taken. This more clearly shows the blood vessels within the brain.
Management options will be made according to the results. This will involve a discussion with the expert team.
Treatment
The aim of your treatment is to prevent another bleed. Recovery from the pain and symptoms takes time as the blood from the haemorrhage is naturally re-absorbed.
After your diagnosis:
Once you have been diagnosed with a subarachnoid haemorrhage, you will be required to undergo bed rest (before treatment) and will be closely observed in the ward environment. Your family will need to bring toiletries and bed clothes plus cordial if you wish. Sunglasses may help if the light hurts your eyes. You can walk about after your treatment if you are well enough and able to although we won’t recommend it if your symptoms are severe.
You will normally be required drink plenty if safe to do so or you will be given fluids via a “drip” into one of your veins. We will also need to measure your urine output and so for the first 7-10 days you will be asked to pass urine in a bottle or bedpan to be measured. This is important as people aren’t able to balance fluids in and out normally after a brain haemorrhage and it is important you don’t get too much or too little fluids.
You will normally take a 21 day course of tablets called Nimodipine. These have to be taken 4 hourly and serve to help prevent complications due to the haemorrhage ie spasm of the arteries.
You will be given regular pain relief and made comfortable. Sometimes people need to have a drain inserted to relieve fluid pressure on the brain. Rarely people may have seizures following a haemorrhage and might require medication.
If an aneurysm is found to have caused the bleed then it may be treated by;-
1.Endovascular embolisation usually with coils or a WEB device
- Surgical clip.
- Conservative management.
The choice of treatment will be made by your consultant neurosurgeon along with the consultant interventional radiologist and multidisciplinary team.
Endovascular embolisation
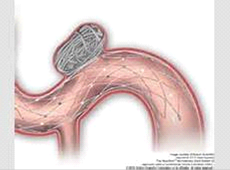
Coil embolisation:
This is an endovascular treatment which means it is performed through
a blood vessel. Under a general anaesthetic, a small catheter (tube)
is inserted into an artery in your groin or wrist in the same way as an angiogram. The catheter is fed up to the aneurysm using x-ray screening. The coils are then deposited inside the aneurysm. The size, shape, and position of the aneurysm will determine which type and how many coils are used. The aim is to pack the aneurysm with coils so that blood is not able to enter it and allow the aneurysm to seal over.
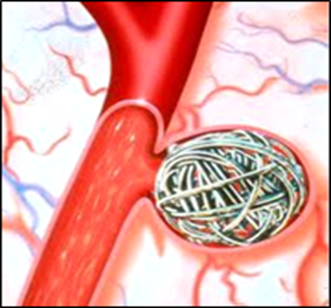
Coils inside an aneurysm
Stent assisted coil embolisation
A stent is a soft, flexible mesh tube made of metal that is placed inside the artery. Stents vary in size and structure: They can be used on their own or with coils to seal off aneurysms.
Stents are usually inserted in a planned elective procedure but on rare occasions, a Stent (artificial tube) is placed in the artery as well as coils to help seal off a ruptured aneurysm. This would depend on the type, shape and position of the aneurysm. Certain types of stents are used on their own.
WEB occlusion of aneurysm
A WEB (or woven endobridge) is a soft, mesh sphere made from braided metal that is placed into the aneurysm and self-expands to seal it off. They come in various sizes and your aneurysm is measured prior to placing to secure the ideal fit.

Other treatments used to seal aneurysms
This area of medicine is continually improving and new devices may be used
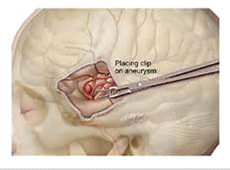
Surgical treatment by clipping
This involves placing a small metal clip around the base of the aneurysm to seal it off and so prevent further bleeding. The operation is done under general anaesthetic and carried out by a neurosurgeon. Part of the hair may be shaved. A cut will be made in the skin and bone to allow access to the brain and the aneurysm. The surgeon will then locate your aneurysm and seal it off by placing a clip (or clips) across the neck (the part where the aneurysm joins the artery) to seal off the aneurysm. The bone will be replaced using small plates after surgery and the skin stitched or clipped up.
The neurosurgeon checks the aneurysm is fully sealed at the time by using a specialist dye through the artery.

Conservative management
Depending on your current health, the position and size of the aneurysm and the risks of treatment versus the benefits, it may be decided to manage the aneurysm ‘conservatively’. This means that symptoms will be treated and the aneurysm will be monitored.
After treatment
After your aneurysm is treated, you will often spend the first night or two in the critical care unit (HDU / ICU) on the ground floor. Depending on how you are and what treatment plan has been ordered by your consultant, your stay in critical care may be longer than 24 hours. You will be reviewed daily until you are ready to go back to the wards.
You will normally stay in with us about 2 weeks (longer if your recovery is more complicated or you need specialist rehabilitation).
Once the team at the Walton centre are happy that you no longer need specialist facilities, you will either go home or to another hospital for local rehabilitation. You won’t go home until the team, including physiotherapists, occupational therapists and speech therapists are happy it is safe for you to do so. They may plan further input as an outpatient closer to home if needed.
Follow up
Your follow up will be at the Walton Centre or another neurosurgical unit if that is closer to where you live.
You will normally be seen 2-3 months after going home for review.
If an aneurysm has been treated by endovascular means (for example with coils) you will normally have follow up by MR scanning although some devices require an angiogram. The MR scans are generally at 6, 18 and 60 months afterwards although this can change according to individual circumstances.
In some cases, a plan is made to come back for further treatment at a later stage: this could be second stage treatment of the aneurysm that has bled (for example with a stent) or to treat other aneurysms that haven’t bled. This is usually planned for when you have recovered from the subarachnoid haemorrhage (about 6 months later)
If an aneurysm is clipped, you will need a follow up angiogram: this is sometimes done before you go home but more usually after a few months.
You will be reviewed after 2-3 months, and plans will be made for the angiogram at that time. If you are well with no other aneurysms then you are usually only seen once more to check on your progress and answer any questions you may have although this can also change according to individual circumstances.
Complications after SAH
The aneurysm that has bled is sealed off to prevent another bleed: it doesn’t prevent complications you may have as a result of the blood in your brain. Whilst these complications are real; you will be monitored closely in the expert centre so that they are noticed and acted on early.
Hydrocephalus
Hydrocephalus is a condition where there is a build-up of cerebrospinal fluid (CSF) in and around the brain and spinal cord. This happens because it may not be able to drain away after the haemorrhage. Hydrocephalus can occur acutely after the initial bleed or whilst you are in hospital or less often, slowly after you have gone home.
Treatment for hydrocephalus includes an external ventricular drain (EVD) which may need to be inserted urgently whilst you are in hospital or a Lumber drain in the spinal cord.
If it becomes evident you need more permanent draining of the CSF you will need a shunt which is a more permanent drainage tube that allows the fluid in the brain to be drained into the sterile cavity in your abdomen.
Symptoms include a build-up of headaches, increasing drowsiness, problems with balance, possible problems with passing urine (incontinence) and possibly worsening vision and memory/concentration (more obvious than when you left hospital) These symptoms must not be ignored. If they are getting worse, you must go to your nearest accident and emergency department for a scan or let us know. Hydrocephalus can be treated by a shunt.
If you have a shunt, you should have information on it.
Support and information on shunts is available.
You cannot drive for 6 months if you have had a drain or shunt inserted.
Spasm of the arteries (vasospasm)
The blood in the brain can be irritable to it. This can, in a few situations cause the blood vessels in the brain to go into spasm. This means that the blood flow (plus oxygen and nutrition) to the brain will be restricted. This can occur in any part of the body but is usually confined to one part or the whole side of the body following a subarachnoid haemorrhage. This can range from a slight weakness to a complete lack of ability to move, talk. It generally occurs after about day 3 and generally the risk subsides around day 10-14. It may be permanent or get better. This is the reason you must stay in the hospital for so long even if you feel well.
Sadly the risk cannot be taken away but it can be reduced by ensuring you drink plenty (or have fluids via a drip) and you take the nimodipine tablets. You will be closely watched, have regular blood pressure and other checks, blood tests and will need to stay in part of the ward where you can be easily monitored.
The nurses and doctors are trained to notice any changes. Sometimes you may need to return to the intensive care for specialist management to try to reverse any complications.
Stroke like symptoms
Sadly, some people have stroke like symptoms as a result of the initial bleed or complications of it: if this is the case you will have specialist rehabilitation which will include support from an expert team depending on your needs
Rarely people get symptoms once they go home. If this happens to you, you should go to your nearest accident and emergency department immediately.
Epilepsy or “fits”
Rarely people who have had a subarachnoid haemorrhage develop epilepsy causing “fits” or “seizures”. The risk is small but at its greatest in the first 6 -12 months after subarachnoid haemorrhage. One fit does not mean you have epilepsy. If you have a seizure, you and your family will be taught safety advice and you may have to take anti-epileptic medication. This should never be stopped abruptly (unless it is only prescribed for a short time such as 2 weeks)
Epilepsy is treated with medication. You will normally be reviewed by a neurologist to ensure appropriate management.
If you have had seizures, you have to inform the DVLA and cannot drive until advised. We can speak to you about this before you go home.
Hair loss:
Very rarely small patches of hair loss can occur after any treatment involving x-rays. The hair usually grows back.
If you do lose some hair, you should use gentle shampoo only and not use strong chemicals such as dyes, perms and strong hair products
If this happens to you, you should let us know
Going home
You and your significant other will have a discussion with the neurovascular specialist nurse before you go home (or to rehabilitation) to talk about your recovery. Please ask your ward nurse to contact us or call on the number advised in contact details.
Medication:
Nimodipine
You will normally be required to complete a 21 day course of Nimodipine at home if it wasn’t completed in hospital. This is just one 21 day course – no more! It is used to reduce the risk of developing complications with vasospasm (a process where the blood vessels close after a brain haemorrhage). This risk has normally passed by 21 days and so the course doesn’t have to be continued. The tablets need to be taken regularly every 4 hours.
Side effects of Nimodipine are low blood pressure, flushing, changes in heart rate, headache, feeling sick and feeling too warm. Please read the leaflet accompanying the medicines given to you to take home from hospital. If these side effects occur, seek medical advice.
Don’t take alcohol or grapefruit juice whilst taking Nimodipine. If you miss a dose by an hour, it is safer to skip it rather than take two doses too close together and so we recommend you set an alarm.
You should get your blood pressure checked once the course has finished as your GP will need to make sure it is well controlled.
Aspirin:
You may go home with a course of Aspirin but only if you have had your aneurysm coiled. Aspirin can sometimes worsen indigestion or heart burn, and may make breathing worse in those with asthma. Occasionally, it can cause bleeding or skin reactions. If these side effects occur seek medical advice. Unless you are taking it for another reason, you should stop it on the date we advise.
Clopidogrel:
Clopidogrel is sometimes prescribed to prevent complications of a coiling procedure. It can cause stomach upset and bleeding problems. If you get excessive bruising or bleeding please contact your G.P. and contact us for further advice. You may need a blood sample taken to check on your blood clotting if this happens.
Pain Relief:
You may go home with pain relief. You should take these regularly to begin with if you need them. They should be cut down as soon as you are able to after the first few weeks as taking them for too long may make headaches worse not better! Certain types of pain killers can cause constipation so please take the laxatives if they are given to you and eat a diet that is high in fibre and don't get dehydrated!
You should aim to be off all regular pain relief by 4 weeks after going home. This doesn’t mean you cant take it occasionally for a bad headache!
You may be more prone to get headaches which is common after subarachnoid haemorrhage; if your headaches persist and are troublesome once you have stopped all regular medication, you should see you GP or speak to your neurovascular team for specialist advice
Sight
Problems with vision such as blurring, blind spots, black spots and double vision can occur following a brain haemorrhage. If this occurs, you should tell your doctor or specialist nurse so that your vision can be checked. If you do experience double vision, you may find it more comfortable to wear an eye patch over one eye. However, for the majority vision settles down after 6-8 weeks.
For some eyesight may deteriorate a little after a SAH. This may improve and so we recommend you do not pay for new glasses in the first 6 weeks after going home if you can manage. Some people need a change to prescription or glasses they didn’t need before after a SAH.
Tersons syndrome
Rarely, the subarachnoid haemorrhage can sit within the fluid in the eye(s) causing changes to vision or even loss of vision in serious cases. With prompt diagnosis and treatment this can (but not always completely) be reversed with a small operation to drain the blood. You should let someone know if you are experiencing changes to your vision to the extent that you are losing patches or all of your visual field.
Communication Problems
The processes in the brain that control communication (i.e. speaking, listening and understanding) may be disturbed following a brain haemorrhage. If this happens, and is problematic, you will normally be referred for speech therapy. Sometimes, but not always, your
speech and ability to understand improve with time.
Memory
It is not unusual to be left with poorer memory following a brain haemorrhage. Your memories before the haemorrhage will be less likely to be affected. This may improve with time but recovery can be frustrating as often your memory and concentration aren’t as good as before. Try breaking down tasks into smaller steps and using a notice board or notebook to help you. Keeping your home organised and making lists helps. If this problem is affecting your day to day life, you may need to be referred for rehabilitation as an outpatient.
Personality Change
Anything going wrong in the brain can cause a change in character or personality. This is especially so with certain aneurysms because of their position. Character changes often settle down or are adapted to with time. If they are on-going and troublesome, you should be referred to a psychologist for an assessment and treatment plan to help you cope. Recovery from any brain injury can take up to 1 -2 years, this will not normally be done until you have been given time to recover (usually about 3-6 months after).
Extreme tiredness
You will probably need rest once you get home particularly if you are having a lot of visitors or your house is very busy. Even simple tasks such as a walk to the local shop may leave you feeling exhausted. This will improve with time but may not go completely. You will know if you have done too much as you will be exhausted and may experience headaches. This often happens early evening or the next day and means you must rest! You should aim to have a rest each afternoon when you go home. Keep this for as long as you are benefitting from it.
Headaches
Headaches are common after a subarachnoid haemorrhage. They usually ease with time. They may, however, persist. Headaches can be triggered by dehydration, stress, illness, too much or too little sleep and missing meals. Prolonged or regular use of analgesia (paracetamol, ibuprofen, codeine, morphine etc.) may also worsen or prolong headaches so should be used sparingly and stopped if no longer required. Drinking 2 to 3 litres of water per day, regular meals, ensuring a good sleep pattern and in some instances avoidance of certain triggers (caffeine, alcohol, cheese etc.) can help reduce the frequency and severity of headaches. There are also some treatment options such as menthol sticks to rub on the forehead which may help. Drinking more water and using pain relief at the start of a headache may also help.
Headaches are often worse if you have done too much that day or the day before.
If they persist despite you doing the above measures, then you may need help from your G.P. or a headache specialist
Back Pain and other symptoms:
At the time of a subarachnoid haemorrhage, blood escapes from the artery into the fluid compartment of the brain called cerebrospinal fluid (CSF). This fluid travels around the brain and down the spinal cord in the subarachnoid space.
The blood should not be there and so it irritates the brain causing headaches as well as light hurting your eyes, sickness and sore neck.
In addition, when the blood travels down the spinal cord (usually when you start walking around) it can irritate the base of your spine and cause pain. Sometimes this can be severe and require regular or new medication to help. The pain usually settles down after a few weeks. If it does not, you should let your GP know.
Pacing
You will benefit from pacing our activities when you go home. Exercise will support your recovery and so we recommend a daily rest as well as some gentle exercise. Build up activity as you feel able and try to go outside for regular walks if you are able, otherwise you may lose your confidence. Exercise can be built up gently but we don't advise ‘extreme’ exercise until after your 6 month follow up scan has been reviewed.
Unusual sensations
Some people experience unusual or strange sensations in their head following a brain haemorrhage. We are not sure why this occurs, but do not worry about them and they should ease with time.
Fear of rebleed
This is a very common fear for all patients as you cannot see inside the brain and SAH usually occurs without warning. Unfortunately, the risk is real but it is very small. However, because the aneurysm cannot be taken away, it is important to learning a coping strategy as this fear may prevent your recovery progressing. Remember, you will be followed up and scanned regularly once you have gone home. You will only be discharged from the Walton Centre when we think it safe to do so.
Changes to smell and taste
You may lose your sense of smell (and taste) after a brain haemorrhage. This usually (although not always) improves with time.
Sensitivity to noise
This is not uncommon following a brain haemorrhage. Everyday noise such as television or background conversations can be just as difficult to cope with as loud noises. This usually settles down with time as you recover.
Recovery is dependent on how you feel. You will need to pace activities for the first month or more after going home because of tiredness and headaches. Feelings of anger, frustration and sadness are not uncommon following a brain haemorrhage. This may be due to the condition but could just as well be due to the sudden life changing event and so will usually pass with time. Getting regular exercise and fresh air as well as eating well may help with mild symptoms. If you are feeling low, you should talk to your GP. You may need to be referred to a psychologist or you can self-refer to local talking therapies in order that you are able to manage.
Enlisting the support of the “Brain Haemorrhage Support group” affiliated to the Walton Centre or the Brain Charity may help in that they may be able to offer emotional support and recovery advice. They are people who have been where you are now and so are a valuable source of support.
However, not everyone is affected this way; some see this as a new beginning; a time to re-evaluate their life following the trauma.
Using a diary from when you are in hospital and for the following weeks or months can be very useful. By charting good and bad days, you will be able to mark your progress; this will help a lot when you have ‘bad days’ and will mark how far you have come with recovery.
Everyday Activities
Driving
Following a subarachnoid haemorrhage, if you hold a driving licence, you are legally required to notify the Driver and Vehicle Licensing Agency (DVLA). You will not be able to drive until you have received DVLA approval and your doctor has confirmed you are recovered. If you drive without telling the DVLA, then your insurance becomes invalid.
This is because driving involves many different cognitive and physical skills as well as multi-tasking, decision making and problem solving.
Driving restrictions are enforced by the DVLA and each case has to be approved individually. You must speak to your medical team or nurse to clarify driving restrictions.
Flying
If you have had a coil occlusion of your aneurysm, you should be able to fly as soon as you feel able. However, if you have had surgical treatment then current advice is to wait for 6 weeks unless your doctor advises you otherwise. It is safe to go through the metal detectors in the airport. They will not affect the coils or clips.
Drinking Alcohol
Don’t drink alcohol until the 21 day course of Nimodipine is completed and you have reduced the number of pain killers you take. However, most people find they are not able to tolerate large amounts of alcohol following a brain haemorrhage. The government suggests that woman
do not drink more than 2-3 units each day and men 3-4 units a day. Information websites on alcohol awareness is printed at the back of this booklet
Smoking Cigarettes
As cigarettes are one of the biggest risk factor in causing an aneurysm to rupture, it is advisable that you give up smoking completely. A free help line number is printed at the end of this booklet.
Returning to work
You can return to work as soon as you feel able from 6 weeks following your brain haemorrhage. However, most people need about 3-4 months, to recover. (Occasionally longer if there have been significant problems)
It is advisable to go back to work on a phased return.
This means you build up your working days and hours according to how you are feeling. A phased return is often graduated over 4 weeks or longer and your employer has an obligation to adhere to it.
Access to work or the Brain Charity may be able to help you if you are having problems with your employer who has a legal responsibility to make reasonable adjustment to support you as you recover. The number is printed at the end of the booklet.
Sexual Activity
You can resume sexual activity as soon as you feel able.
Starting a family
It is advisable not to start a family for the first 6 months following your brain haemorrhage as it takes this time to recover. You will not normally be prevented from a normal delivery but this will depend on your obstetrician. You will not normally have MRI scans whilst you are pregnant. Please talk to us for further advice if you become pregnant.
Sport and swimming
As long as wounds have healed, there is no problem with swimming. However, it is advisable to go with somebody (or let the life guard know) during the first year following your brain haemorrhage because of the small risk of seizure. Most other sports can be resumed once you have recovered. Exercise is encouraged as it improves stamina and wellbeing. However, you should build up your fitness slowly as soon as you feel able and we don’t recommend extreme exercise until after your 6 month MRI scan results.
Hair Washing
If you have a head wound, this can be done after 48 hours. It may be more sensitive to fluctuations of temperature. Always test the water temperature before washing. If your aneurysm has been coiled then you can wash it as soon as you feel up to it.
Reassurance about coils
Coils are fixed in place. They are not affected by airport security scanners, microwave ovens, magnets nor mobile phones.
Hair Dyeing
You can dye your hair once the wound has healed completely and the hair grown about 2 inches if you have had surgery. The skin around the surgical site may be more sensitive for some time afterwards. You can dye your hair as soon as you feel up to it if your aneurysm has been coiled.
Dental Treatment:-
Dental treatment is safe after SAH. If you have had surgery you may find you have a pain in your jaw for the first few weeks when opening your mouth or chewing and may benefit from postponing it until you feel more comfortable.
If you have had an aneurysm coiled and treatment isn’t urgent you should wait until the aspirin finishes or consult your dentist and contact us for further advice.
Family and friends
Enlist the support of your family and friends whilst you recover. They will be a great help with shopping, transport and support if you feel down. Family and friends support is helpful during the first 4 weeks after you go home and will be the biggest influence in your successful recovery.
Making time for them will be beneficial in your recovery. If you aren’t feeling so confident just make plans for short visits or regular texts so that you don’t lose touch
Where can I meet other people who are going through similar
experiences?
There are details of the brain haemorrhage support group, and other links you may find useful in contact details at the back of this booklet.
Will I be entitled to any benefits?
You may be entitled to sick pay from your employer, or you are likely to be able to claim benefits appropriate to your specific situation. You should contact a charitable agency such as Citizens Advice Bureau, Welfare Rights or Brain Charity to discuss individual circumstances and what you are entitled to. Access to work accessible through https://www.gov.uk/access-to-work
Going home information
Name:
Consultant:
Date of Sub-Arachnoid Haemorrhage:
Date and type of treatment:
Follow up advice:
- See your GP for blood pressure and cholesterol check about a month after going home unless advised otherwise
- Pace your activities for the next few weeks- months depending how you are feeling. This includes gentle exercise starting with a short walk to build energy and stamina: once you can manage half an hours walk , 5 days a week you can start gentle exercise and build up gradually as/ if you are able: No extreme exercise is advised until after the 6 month MR scan.
- You will benefit from taking a rest each afternoon for the next few weeks
- You should keep your energy for the things you want to do and the things you have to do as if you do too much you may find you become exhausted later the same day or the following day
- Keep hydrated, not missing meals, not getting too much or too little sleep will support your recovery and help with headaches and fatigue (about 2 litres should be OK)
- If you smoke you should consider giving up as this is the biggest known risk factor in aneurysm formation: you can get help from your GP and local smoking cessation services
- You should not drink alcohol in excess
- More specific advice including headache management is in your information leaflet on subarachnoid haemorrhage
Driving restrictions: Driving is a complex task requiring multiple skills. For that reason, the law requires you MUST inform DVLA and you cannot drive until you are recovered and have clearance from them
- Driving restrictions differ from person to person and are dependent on what you have had done; how the brain haemorrhage has affected you and how you recover
- Specific driving instructions:
Working: Most people need 6 weeks - 3 months to recover- Get as much help as you can for the next couple of months whilst you recover
Access to Work- https://www.gov.uk/access-to-work gives advise and the Brain Charity - https://www.thebraincharity.org.uk can support you when you go back to work
Medication:
- Nimodipine 60mg 4 hourly (usually 10, 2 and 6 o’clock) to stop– you should not take this with alcohol or grapefruit.
- Aspirin 75 mg once daily to be taken half an hour after food until
You may need to take pain killers regularly for a couple of weeks but should aim to be off regular painkillers a month after going home although you can take it if you get a headache. This is because long term regular use of regular pain killers can make headache worse.
After a month your headaches should have improved. If they continue regularly and are troubling you we advise you call as you may need specialist advice.
If you suffer from any side effects of the medication we prescribe please let us know and see your GP
Appointments:
- See your GP for a blood pressure review within 1 month of going home
- Phone call to check on your wellbeing: (usually between 4 and 6pm)
- Nurse clinic 2-3 months
- MR scan follow up usually 6, 18 and 60 months
- If you have any questions call the nurse helpline on 0151 556 3325
- Last Updated:27 January 2023
- Review Date:27 January 2025
- Author:C Stoneley, Neurovascular ANP
- Summary:
What is a subarachnoid haemorrhage and the treatment for it