Surgery to remove a brain cavernoma
What is a cavernoma?
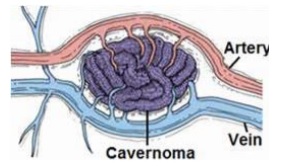
A cavernoma is an abnormal cluster of dilated blood vessels that look small bubbles described as caverns. The caverns are filled with blood that makes them look like a blackberry. These can be in the brain or spine and range in size from tiny to up to several centimetres in diameter.
There isn’t a lot of blood flow inside a cavernoma, but the walls are weak and so blood can leak out and cause symptoms.
Some cavernoma are associated with other vascular abnormalities (or variants) such as a venous anomaly
Incidence of cavernoma
Cavernoma occur in approximately one in 200 of the general population.
The majority of people with cavernoma have only one lesion and no family history meaning they are sporadic and not usually inherited
If you have more than one cavernoma or someone else in your family has been diagnosed with one as well as yourself it is reasonable to suspect a genetic component. If this is the case, you may be offered or request genetic counselling to evaluate your family’s risk of cavernomas. There are three known genes associated with cavernoma formation
If you have the inherited form of cavernoma, each of your children has a 50 percent chance of inheriting the condition
Where do cavernoma occur?
Cavernoma generally occur in the brain and spinal cord
Many are there at birth and some develop later in life
What are the possible problems associated with having a cavernoma?
The type and severity of the symptoms depends on the size and location of the cavernoma.
Some people have completely incidental cavernoma which cause no symptoms. In some people, however, cavernoma can cause haemorrhage or bleeding in the brain.
Adults are more likely to have symptoms from cavernoma although they do occur in children.
In some cases cavernoma can irritate the brain and cause seizures, stroke like symptoms, bleeds, changes in vision, balance problems, swallowing problems, headaches and or spinal cord injuries. Symptoms vary depending on where they are in the brain and how the symptoms affect you individually.
Rarely, they can cause cognitive changes or impairment of memory or a build-up of fluid in the brain called hydrocephalus
Some locations of cavernoma are more dangerous than others in that they may cause more damage/problems when they bleed
Why treat a cavernoma?
Treatment for cavernoma is generally done because you are having symptoms from it. The decision to treat is made with your neurosurgeon who takes into account your well-being and personal wishes.
The most common reason for surgery is to reduce the risk of seizures or if you are having progressive symptoms of stroke or because the cavernoma is repeatedly bleeding and causing problems
Once a decision is made and discussed with you by your medical team; with your agreement you will be placed on the waiting list for treatment.
Preparing for the operation
You will be seen in the pre-operative clinic and your fitness for a general anaesthetic will be assessed. At this time (or a phone call with the neurovascular nurses will be planned) the procedure will be discussed, and any concerns answered. You should allow 1 ½ - 2 hours for this appointment.
Please bring a list of your medicines and a urine sample to your pre-operative assessment. Bloods and measurements of height and weight will also be taken.
Further tests may be necessary according to your general well-being and other medical conditions before a decision is made that you are fit for the anaesthetic procedure.
You will be assessed by an anaesthetist before the operation. The anaesthetist is the consultant doctor who administers the general anaesthetic and pain relief during the operation. This is usually done when you arrive at the ward but if you are considered higher risk; this may be done as an outpatient.
You should shower and wash your hair in the solution given to you in pre-op, as advised before the operation in order to clean the skin and reduce the risk of infection.
You normally come in the same day as the planned surgery. You should present to your designated ward at approximately 7:00am ( or the instructed time) on the day of your operation.
You should not eat anything from midnight but you can sip water only (no other liquids).
You will stop any blood thinning medication prior to your operation. Your pre-op nurse will instruct and advise you which medications to stop and for how long. All other medication will be taken as normal.
Surgical excision of the cavernoma
The operation will be carried out whilst you are ‘asleep’ under general anaesthetic which means you will not be aware or feel anything.
The operation is carried out through a craniotomy. A craniotomy is an operation to remove a window of bone in the skull to expose the brain.
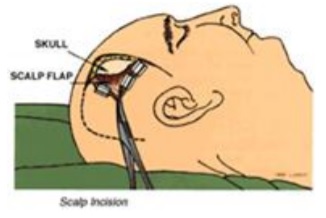
Once asleep your head is stabilised; in some cases, a small amount of hair may be shaved. If possible, this will be behind the hair line. An incision is made in the skin to expose the bone. Small holes called burr holes are made in the skull bone and the surgeon uses these to form and take out a window of bone called a ‘bone flap’. The bone flap is temporary and necessary to expose the brain underneath.
The brain is covered in a lining called the dura. This is opened and the surgeon locates the cavernoma through the natural folds of the brain using a microscope. The cavernoma is visualised and carefully excised.
Once the surgeon is happy the cavernoma is completely removed the bone flap is then put back in place and secured using tiny metal plates and screws. The skull itself will take about 6 months to heal. You may be able to feel the indentations from the burr holes once the wounds heal. This is normal.
After the procedure
Once the operation is over you will go to the post-operative recovery unit to wake up and recover from the anaesthetic. You will be looked after there by skilled post-operative recovery nurses. Once you have woken up and been assessed by the anaesthetist, you will be moved to a ward or the high dependency unit. Where you go depends on how quickly you wake up, how long or complicated the procedure was and other medical conditions you may have. The high dependency unit is used to monitor you more closely if needed but it is likely you will go back to a ward.
You will have a drip in your hand or arm to give you fluids through a vein.
You will have a bandage on your head and you may have a drain under the skin in the head.
You may have stockings or compression devices on your legs to prevent complications such as deep venous thrombosis (DVT). DVT is a blood clot in the leg that is at risk of occurring when you can’t move around as much as normal.
Observations will be done of your blood pressure, pulse, respirations and you will have your consciousness level and pain assessed.
Recovery
There is a small risk that the area of brain near to the cavernoma will be affected afterwards. This may be short term because of swelling or bruising but in rare cases can have a long-term effect.
Bruising around the face and swelling to the eyes is common. This settles in several days to a few weeks but can be uncomfortable and painful. Regular pain relief can be given to help these symptoms.
If the eye is affected, it should be kept clean to prevent infection.
Pain/headache following this operation is expected. You will be prescribed regular pain killers. The pain is due to the surgery. This is normal and eases with time.
Your surgeon is likely to let you home once you are up and about and pain is well controlled.
Recovery can sometimes take longer if there have been complications because of the operation or afterwards and you need some rehabilitation. There is a very small risk of complications that may lead to a second operation.
As the wound heals the stitches can feel tight; this settles after the stitches are removed. The pain from the operation may persist for a few weeks to months, although will be less severe.
In the early stages, the area around the wound feels numb. This is because the nerves have been cut. As the nerves grow back there is abnormal sensation such as pins and needles which settles over several months. The wound may itch as it heals. Please do not scratch it as you will risk infecting it.
There is a very small risk the wound site may become infected. It is rare because you will have cleaned the head and hair before you come in and antibiotics are usually given at the time of the operation. You must not touch, scratch or pick at the wound as this will increase the risk of infection.
If the wound becomes, sore, inflamed, red, oozes or you get a temperature when you go home then you should get in touch with your consultant, ward and/or neurovascular nurse for a wound check and assessment including bloods to look for infection.
The muscle that is used for chewing food can be affected in some cases as this may be bruised, cut or swollen as a result of the surgery. As it heals the muscle may shrink causing difficultly in opening the mouth or chewing. These symptoms usually settle within 6 months.
The bone flap (the piece of bone cut out during the operation) might feel like it moves; the pressure in your head varies and this makes it feel like the flap of bone moves in and out but it is secure. You might also experience a “clicking” sensation. Although this feels strange, it is not dangerous. The bone flap is not loose: it is secured when it is replaced and will heal. If you have any concerns regarding the wound or bone flap you should let us know.
Pacing
It is advisable to pace activities for the first few weeks following going home. This will be so that you don’t get over tired which may slow your recovery. Enlist the help and support of your family and friends to help with household chores if you can. Take some gentle exercise to help build up your stamina each day, for example a short walk building up as you get stronger. You may also benefit from an afternoon rest for the first couple of weeks after going home.
In the initial stages, your recovery and headaches will benefit from keeping a regular routine ie going to bed and getting up at the same time each day, not missing meals and keeping hydrated.
Working
Full recovery can take a few months which means you may have to allocate time off work. The time off work depends on the type of job you do and your level of responsibility. Most people need about 2-3 months.
If you have to go back sooner for financial or other reasons, this won’t do you any harm but it sometimes takes you a bit longer to recover as you may feel more tired.
You will normally go back to work on a phased return which means your employer has an obligation to build up your hours gradually and assesses your progress. You can get useful information for returning to work on the government’s access to work website detailed at the end of this booklet
Driving
Driving involves many different cognitive and physical skills as well as multi-tasking, decision making and problem solving. The DVLA currently states you must inform them if you have had surgery for a cavernoma and current guidance states you cannot drive for 6 months if the cavernoma is in the top portion of your brain (supratentorial) and driving after that will depend on your recovery. If the cavernoma is in the bottom portion of the brain (infratentorial) you must still inform the DVLA after surgery and driving will depend on your recovery and any ongoing impairment that may affect safe driving.
Driving restrictions are enforced by the DVLA and specific to the position of the cavernoma, the treatment, symptoms from it and whether it has bled or not.
If you have seizures, you must not drive until you have been seizure free for 12 months.
Other symptoms such as stroke like symptoms and changes to vision may affect your ability to drive.
You must speak to your medical team or neurovascular nurse to clarify driving restrictions
Driving regulations change all the time so please check with your doctor or nurse before going home from hospital
Headaches
If your headaches started after a bleed or treatment then they may ease with time. Headaches can be triggered by dehydration, stress, illness, too much or too little sleep and missing meals. Staying hydrated will help reduce the frequency and severity. Also, try and get back to a normal sleep pattern as soon as possible and don’t miss meals.
Try putting some structure into your day, including meal times as this will help with headaches and recovery. Stopping smoking and reducing the amount of caffeine you take may help reduce the severity of headaches.
Menthol sticks to rub on the forehead can help. Drinking a pint of water at the start of a headache may also help. Taking regular pain medication for a long time can also make headaches persist and so should be reduced as soon as you are able.
If headaches persist and are troublesome you may need specialist management.
Hair
You can wash your hair using a mild shampoo after 72 hours. You can dye your hair once the wounds have completely healed.
Sex
You can have sex as soon as you feel able.
Seizures
There is a small risk of seizures after any type of brain surgery. The position of certain cavernoma can carry a bigger risk of seizure.
Surgery for cavernoma is sometimes done to prevent seizures: there is an approximate 80% chance the surgery will stop seizures, but your neurosurgeon will be able to let you know the specific number as it is individual to each person. You will normally stay on your anti-epileptic medication after surgery and discuss stopping it with your doctor if you have been seizure free for a specific length of time as advised by your neurosurgeon.
Stopping seizure medication carries a risk of recurrence of seizures; for that reason, if agreed with your consultant you should not stop medication abruptly but reduce it gradually, often over a few months. Stopping medication has driving implications which means you cannot drive whilst you are reducing medication and for 6 months afterwards.
Flying
It is advisable not to fly for six weeks after your operation. Following that it should be fine but should tell your insurance company.
Exercise
You can build up your exercise regime gradually as you feel able once you have recovered from the operation. Do not do any extreme exercise for the first few months in order to allow the bone and wounds to heal. You should avoid contact sports after surgery and may need to wear protective head gear if you pursue this once recovered (speak to your nurse or consultant before embarking on any contact or extreme sport).
Alcohol
It is advisable not to drink alcohol until you feel recovered. If you have seizures, excessive alcohol can lower the seizure threshold and make you more susceptible to having them.
Smoking
It is advisable that you do not smoke. Smoking cessation clinics are linked to every G.P. Practice or you can ask for help during your stay in hospital. An advice number is printed at the end of this leaflet.
Follow up
You will normally be reviewed after 2-3 months to check on your recovery.
You will normally have an MR scan to check the cavernoma is completely gone. If it has then you will not normally need any further follow up unless there have specific problems or there are other cavernoma.
Self help
Cavernoma alliance UK offer practical advice and support for people who have cavernoma.
Walton Centre Contact Details
For any emergency please attend your local
Accident and Emergency Department or see your G.P.
Patient Experience Team provides a PALS service. 0151 556 3091/3090/3093 wcft.patientexperienceteam@nhs.net
Neurovascular Nurse Specialists: 0151 556 3325 (Non-urgent advice or enquiries).
Walton Centre switchboard - 0151 525 3611
- Dott ward - 0151 556 4276/3887
- Cairns ward - 0151 556 3567/3568
- Caton ward - 0151 556 3588/3894
- Caton short stay ward – 0151 556 3576/3568
- Chavasse ward - 0151 556 3897 / 3591
- Lipton ward – 0151 556 3344/3383
- High dependency ward - 0151 529 5489
- Intensive Care Unit - 0151 556 3462/3798
For information regarding appointments or DVLA please contact your
consultants secretary.
Useful Contact details
NHS 111: 111
Telephone advice if you need urgent medical help fast but it is not a 999 emergency (or you do not have a GP)
Website: http://www.nhs.uk and search
‘emergency and urgent care’
D.V.L.A. Driver Vehicle Licensing Authority,
Drivers Medical Group, DVLA, Swansea, SA99 1DL.
Medical Enquiries: 0800 032 5202
Access to work. https://www.gov.uk/access-to-work
The Brain Charity: 0151 298 2999.
Offers practical help, emotional support and social activities for people with neurological injury. And their families/carers
BASIC Manchester: 0161 707 6441
https://www.basiccharity.org.uk
(Similar to Brain Charity if this is closer for you).
Cavernoma alliance: 01305 213876 www.cavernoma.org.uk
Brain and Spine foundation: 0808 808 1000
NHS Free smoking helpline: 0800 0224 332
England: 0300 123 1044 Wales: 0800 085 2219
Advice on Alcohol: 020 7766 9910
- Last Updated:02 May 2023
- Review Date:02 May 2026
- Author:C Stoneley
- Summary:
What is a cavernoma and the treatment for it