Thoracic Spine Surgery
Welcome to the Walton Centre
Admission to hospital can be a daunting experience for most people. The information in this booklet is designed to help you understand what will happen to you during your time with us. It also contains your physiotherapy exercises for you to do following your surgery and some general advice following your surgery.
This booklet contains information about thoracic spine surgery. There is an explanation of some terms that you may hear. If you have any questions before or after your surgery, then please contact us via the contact details below.
For further information please see patient information on British Association of Spine Surgeons website (spinesurgeons.ac.uk/Booklets).
How is the spine constructed?
The spine is constructed in two parts, the spinal column which consists of the bones (your back bone) and the spinal cord which consists of the nerves of the spinal cord that pass messages through from your brain to your body and back again.
Spinal column
The spine is composed of small bones called vertebrae which all sit on top of each other to form your spinal column. The vertebrae get larger as they go down the spinal column, with the largest being in the lumbar (lower back) region.
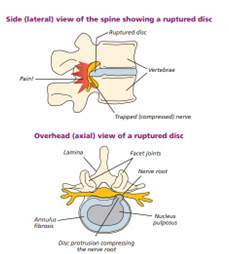
To stop these bones from rubbing on each other you have intervertebral discs. These are soft cushions of tissue, which sit in between each of the bones in your spinal column and act as shock absorbers, stopping the bones from rubbing on each other.
There is a tough band of elasticated tissue called the ligamentum flavum, that helps the stability of the spine by connecting the bones together.
The spinal cord and nerves are protected by a thin layer of tissue, called the dura mater, and this contains the fluid, called CSF, that surrounds the nerves and spinal cord.
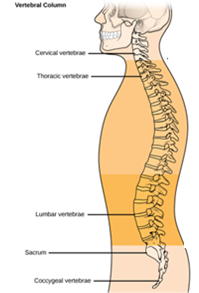
Spinal cord
The spinal cord consists of millions of nerve fibres which run through the middle of your spinal column. Your spinal cord, and the nerves it is composed of, act in a similar way to a telephone exchange passing information from your brain to your body and back again. At the level of each vertebra your spinal cord sends out one nerve on the right side and one on the left side. These nerves contain hundreds of nerve fibres that transmit messages between your body and brain. The cervical vertebrae are in your neck, thoracic are in your trunk and the lumbar and sacral vertebrae are in your lower back. Any problems with your spinal column that causes pressure on your spinal cord or nerves can cause problems with feeling and/or movement.
Pressure to nerves can be caused by one or a combination of factors:-
Slipped disc/bulging disc
Osteophytes – overgrowths of bone
Ligaments – elastic tissue that can become hard and calcified with age
Enlarged joints – get larger with age, wear and tear
Nonalignment of the bones – often becomes worse with degenerative changes
Why do we perform spinal surgery?
Surgery for problems with the spinal column or spinal cord and/or nerves, can be performed for many reasons. In general, you will have been offered surgery to:
1. Give you relief from pain
2. Stop any further deterioration in the feeling and/or function at and below the affected part of your spine.
3. Give you a chance of making some recovery from any symptoms.
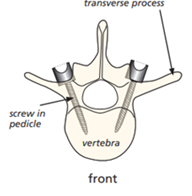
The main aim of surgery is to remove what is causing the pressure on the nerves. It is important that you understand that spinal surgery is often performed in order to prevent any further deterioration in movement or sensation. Metalwork, such as a screws and rods are inserted to stabilise the spine and encourage the bones of the spine to fuse (join) together. If nerves and/or spinal cord have sustained damage, quite often over a prolonged period of time; the damage already caused to the nerves or spinal cord may not be reversible, despite surgery to remove the problem. This is why sometimes weakness, numbness and other symptoms may not improve. Any recovery of symptoms will often take time and can take up to two years.
The following information is to help you understand what we are offering you and why. Please remember, agreeing to surgery is your decision. The job of our team is to present you with the facts and options as we see them. You have the right to change your mind at any point in time, if you wish for further explanation at any time please just ask one of the staff.
Surgical procedures
Thoracic decompression:
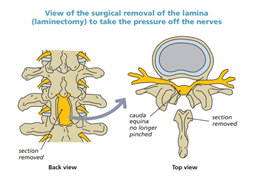
This is a generic term used to describe removing pressure from the spinal cord/ nerves. This usually involves removing some bone to widen the area where the spinal cord passes through.
Thoracic fixation:
This is where screws and rods are used in order to fix the bones of the spine together. This will stop/ reduce abnormal movement of the bone that can cause pain, or problems with the function of the nerves. This surgery may be performed alongside a decompression.
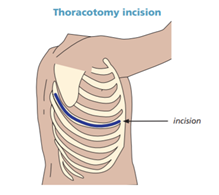
Thoracotomy:
Occasionally whatever is causing compression of the cord cannot be accessed through the back. Your surgeon may discuss a surgical procedure called a thoracotomy. This involves making an incision on the side of the rib cage and in between the ribs. The rib or part of the rib will be removed, and your lung will be deflated in order to allow your surgeon better access to your spine. The part of the disc and occasionally bone will be removed to decompress your spinal cord. You may require stabilisation with metalwork (fixation) also.
What are the risks?
General risks:
- Nerve root injury: this can cause weakness, numbness or pins and needles.
- Spinal cord damage: loss of power and/or sensation in legs, loss of control of bladder/ bowel.
- Dural tear (tear of the lining covering the nerves): this is usually repaired in theatre with stitches, patch or special glue. If the hole reopens then you may get CSF leaking from the wound, headaches or, very rarely, meningitis (an infection of the lining of the brain and spinal cord). If the leak cannot be repaired you may need a lumbar drain, again, very rare.
- Risk of increased nerve pain.
- Risks from positioning during surgery and equipment used, this can include pressure problems, skin injuries, blindness (this is exceptionally rare).
- Infection: this can be at the surface of the wound. If the infection is deep this may require further surgery and a prolonged course of antibiotics.
- Wound drain problems, requiring removal in theatre – very rare.
- Risk of clots in legs or lungs, you are encouraged to move around as quickly as you can and regularly whilst you are in hospital. You will be given blood thinning injections whilst you are an inpatient and given compression stockings to reduce the risk.
- Bleeding: This is expected during the surgery, surgeons will take measures to try and minimise this. Occasionally specialist equipment is used to “recycle” your own blood in theatre. You may require a blood transfusion.
- Lack of fusion.
- If metalwork is used: Difficulty with screw placement or screws breaking, or movement/ breakage of implant/ rods/screws - which may require further surgery.
- Worsening of symptoms despite adequate decompression
- No improvement of symptoms
- Anaesthesia – more information in anaesthetic booklet.
Risks specific to Thoracotomy:
- Build-up of fluid or blood inside chest wall (pleural effusion/ haemothorax)
- Collapsed lung (pneumothorax)
- Fistula – abnormal passage between airways in the lungs – symptoms may include persistent cough or shortness of breath
- Damage to lymphatic system
- Chronic post operative thoracotomy pain – reported in 1 out of 10 cases.
- Build up of fluid within the lungs (pulmonary oedema): treatment may include water tablets to encourage increased fluid output through urine, symptoms may include shortness of breath.
- Respiratory failure - lack of oxygen in the blood leading to poor oxygen supply to your organs.
- Damage to spinal cord: this can result in loss of control and sensation to legs and loss of bladder, bowel or sexual function. This operation may be done with the assistance of neuromonitoring to monitor nerve function whilst you are asleep, this helps to reduce the risk of neurological damage.
Alternatives to surgery
It is your decision if you wish to have surgery and surgery will only have been offered to you if your consultant feels that it may be of benefit to you. If you do not wish to have surgery then your surgeon will discuss the individual implications this will have for you.
Here are some alternatives that may be suggested to you:-
1. Wait to see if your condition remains unchanged without surgery.
2. Manage your pain with analgesia (painkillers)
3. Pain team intervention, to see if they can help manage your symptoms.
4. Physiotherapy can often be effective as a conservative measure
Pre op assessment
In order to gain the information we need to ensure your safety during your surgery, once you have agreed to surgery you will be required to complete a pre-operative assessment online. You will be provided with the information you need on how to complete this. The information you provide will be reviewed by one of the pre op nurses. It is very important that you complete your pre-operative questionnaire with all the details as accurately as possible, as inaccurate information may delay your surgery.
Following this you will be asked to come into clinic to see a member of the preoperative assessment team, an appointment will be sent out to you. At this appointment a member of the team will discuss your medical history including your past operations and any medical conditions you may have and you will be examined. This will include checking your blood pressure and listening to your heart and breathing. You will have blood tests performed. If any x-rays or a heart trace (ECG) are required these will also be done. Please bring a list of you medications and the doses in with you to this appointment. A member of the team will review your medications. It is very important that you tell us about all your medication, including all prescribed medication, medication you buy and any herbal remedies. It is especially important that you tell us about any medication that may thin your bloods. If you need to stop any medications before surgery the team will advise you on what to stop and when.
You will be given an antimicrobial body wash to use prior to coming into hospital which you should use for 3 days before surgery.
You may be reviewed by an Anaesthetist; they will have a chat with you and discuss any relevant medical history and explain what having an anaesthetic will involve. You are asked to come back on another day for this.
Please be patient whilst we complete all of our assessments. Occasionally we need to postpone surgery if your pre-operative assessment indicates that there are more tests or medication needed before we proceed with your surgery. We understand that this is frustrating, but we will not proceed until we have all the information we require to ensure your maximum safety.
It is important that if you have any changes prior to surgery you must let your consultant’s secretary know in a timely manner. This includes:
- changes in pain or symptoms
- if you develop any new medical conditions, or if you are commenced on new medication
- if you are unwell or if you have an infection.
Some patients may not have a pre-operative assessment of any type, this can be for many reasons, for example, you are admitted urgently or as an emergency and there is no time for all of this to be completed. This is not a problem, because everything you need will be done the day you are admitted. Your surgery in this situation is normally the following day. You will not go home overnight.
You should receive a call from the Spinal Nurse Specialist prior to your surgery. This is an opportunity to ask any questions about your operation and afterwards.
Admission to hospital
You will be able to eat and drink up to midnight the night before your surgery and drink clear water only up to 6am on the morning of your surgery. You will then be able to have sips of water only from 6am until you go for your operation. This will be clarified for you prior to your admission. Most patients will be admitted the day of their surgery at approx. 7.15am, having followed the fasting instructions above.
We advise not to bring any valuables with you into hospital as the hospital does not accept any responsibility for their safety.
When you arrive you will be seen in an admission area and then informed which ward you will go to after your surgery.
Day of surgery
You will continue to be kept fasted (nothing to eat or drink, only clear fluids) and you need to wear a theatre gown. We ask that you have a bath or shower the morning of your surgery before you leave home.
Your details will be checked with you on the ward before you go to theatre. You will be wearing a wrist band and have to answer a list of questions, for example, your name, date of birth and confirm that you have removed all jewellery, underwear and make up etc.
You may need back marking which is perform in the x-ray department. This involves an injection of a marker to the affected level within your spine to guide the surgeons in theatre.
You will be collected for theatre and taken to the theatre reception area, where the Nurse will check you details again; whilst this can appear repetitive it is all done to ensure your safety. From there you will be taken to the anaesthetic room, where your details will be checked again. We have a robust safety check list which includes asking you to confirm what operation you are having, your symptoms, which side of the body and where you experience them, do not be concerned, this is for safety only and not because of any queries about your surgery. Once this is done the anaesthetist will give you your anaesthetic medication, and once you are asleep you will be taken into theatre and surgery performed.
The surgery will be performed by the consultant with other members of the team. It is common for x-rays to be used in theatre to assist the surgeon with checking the correct position of the spinal bones and surgical level.
After surgery you will be taken on your bed into the recovery room where you will be monitored whilst you wake up from your anaesthetic. You will then be transferred to the ward after spending approximately 1-2 hours in recovery. Your observations i.e. blood pressure and pulse will be checked regularly, as will your wound and your limb power. Depending on you operation you may need to spend a day or so in the high dependency unit or intensive care. This is so that you can be more closely monitored immediately after your surgery.
An intravenous infusion (drip) will be in your hand until you are awake enough to eat and drink again.
You may require a wound drain which drains excessive fluid/ blood away from the wound. It is a small plastic tube located just beneath the skin that comes out of the skin near wound and is attached to a collection bag. This is often removed day one or two after your operation.
You may have a catheter in which is a tube into the bladder to collect urine.
It is normal to feel discomfort in the wound area after surgery and around the hip area (due to positioning in theatre) but we will manage this with appropriate pain relief medication.
Some patients will have a PCA (Patient controlled analgesia) this is a push button device that allows the patient to push a button, to deliver some pain killing medication into the vein through a small plastic tube with each push of the button. It has a time out switch so that it can regulate the amount of medication delivered. This is often used for the more extensive procedures or where pain control is an issue, and this will be decided on an individual patient basis.
After Surgery
In most cases the day following surgery your drip will be removed, your wound will be checked and if you have a wound drain and/ or a catheter, we will aim to remove it.
Your individual operation will determine your management. Those requiring more extensive surgery may need a couple of days in intensive care, longer hospital stay, and attachments including drips and catheters left in for longer.
You will be encouraged to get out of bed and move around the ward as soon as possible to help prevent your back muscles going into spasm. If your surgery has been more extensive you will be encouraged to sit out in the chair initially then progressing to walking further. Little and often is key after surgery.
If you have a wound drain, removing this requires the nurse to remove the stitch holding it in place and gradually sliding the drain tube out. It is not normally painful and they are usually easily removed. In very rare circumstances the drain may need to be removed in theatre however this exceptionally rare.
You will be seen by a physiotherapist the day after your surgery who will support you with mobilising and give advice on exercises. You will need to bring this booklet into Hospital with you so that you will know what your exercises are and so that the Physiotherapist can complete the individual details for your exercise programme whilst explaining it to you.
Occasionally, if you are managing well you may be able to go home the day after your surgery, more than likely you will be in at least two nights. Those requiring more extensive surgery will be in for longer.
If you have had screws and rods inserted, when you are up and about you will require an x-ray with you standing. This is to check the metalwork position when you are standing prior to you going home.
Specific for thoracotomy
Post operatively you will need a chest drain which helps the lung to re-expand. If this is the case you will spend time in High Dependency Unit, usually one day. The chest drain will usually be removed the day after your operation when your team is happy the lung has re-expanded.
Pain medications
Many patients who come in for surgery have taken pain medication for a long time. Following your surgery your doctor or specialist nurse may recommend that you take a strong opioid medication alongside other painkillers such Paracetamol and your usual medication. This is to help to manage the additional pain from your surgery. We have an acute pain team who we often ask to review you after your surgery in order to try and make you as comfortable as possible. We will not be able to make you pain free, but we want to make sure that you are able to get washed and dressed, move around and get home comfortably.
When you are discharged, as well as your normal medication, you may be given stronger painkillers to take home. It is important that you do not exceed the maximum dose prescribed for you. It is also important that you do not take any other painkillers that have not been prescribed by the hospital at the time of your discharge. This may result in you having too much and cause the risk of severe side effects.
If you were not already taking painkillers before admission to hospital, you should not need to take them for a long time. The additional pain medication, prescribed whilst you are in hospital, is only intended to be short term. As you recover and your pain reduces you will be able to slowly reduce taking the medicines.
Any medication you were taking prior to surgery should not be stopped suddenly and should be reduced slowly in order to avoid unpleasant side effects. Once you have recovered from surgery, after a few weeks, and as your pain settles discuss with your GP a reducing regime for your medication.
Discharge Home
Getting home
Please arrange for a relative or friend to collect you. You will not be able to drive or use public transport. You can go home by taxi if a member of your family or friend can accompany you. If you are travelling in a car, sit in the passenger seat and recline this to make it more comfortable for your journey home. If you are brought into hospital with hospital transport the ward will be able to arrange transport to take you home.
Medication
Medication can be organised for you to take home, if required. Unfortunately, if we arrange medication from our pharmacy then this can mean you need to wait until later on your discharge day for it to arrive.
Wound Closure
Some patients will have dissolvable stitches in place, some will have stitches that need removal, and some may have metal clips. Your stitches/clips will be due to be removed approximately 7-10 days after your surgery (in some cases longer, but this will be clarified with you before you go home). Most patients make an appointment to get this done by their GP or Practice Nurse, you do not need to change the dressing regularly before this. In the rare event that you are housebound and are unable to get to your GP then a district nurse can be organised to check your wound and remove your stitches/ clips if required. The date of your district nurse visit will be given to you before you leave the ward. If you are not going home to your usual address and you are going to stay with someone else you inform the staff to ensure that the nurse comes to the correct address.
Wound Care
Should you have any problems with your wound after your surgery, even if your GP or district nurse are managing this, it is very important that we are also informed as we may need to monitor your more closely. We would like you to contact us if there is any redness around the wound, wound leakage, or are started on antibiotics.
Please phone either:-
Spinal Nurses on 0151 556 3424
Tissue Viability Team on 0151 529 5599
You can shower, but please aim to keep the wound dressing dry until the wound has healed and any sutures/clips have been removed. Do not soak the wound in water i.e. bath or swimming until the wound has fully healed, about 14 days.
Symptoms to report
These are rare however if you develop any of the following symptoms you should seek medical advice without delay:
- Significant pain
- New or worsening weakness in the legs
- New or worsening numbness
- Bladder problems: Difficulty passing urine, reduced sensation to pass urine or urinary incontinence
- Bowel problems: Loss of sensation to pass bowel movement or bowel incontinence
- Poor control of bowel movement.
Things you can do to help your recovery
- Smoking: this can reduce bone fusion, but also can affect breathing, wound healing and can increase your length of stay in hospital. We encourage you to stop or certainly reduce smoking prior to surgery in order to reduce your risk of complications.
- Diabetes: poorly controlled diabetes can also increase your risk of developing an infection.
- Obesity: this can increase your risk with an anaesthetic.
- Malnutrition: You will need adequate nutrition for your body to heal after your operation.
For more information regarding preparing for your operation, please see Royal College of Anaesthetists – Preparing for Surgery, Fitter Better Sooner on https://rcoa.ac.uk/sites/default/files/documents/2022-10/FitterBetterSooner2022web.pdf
Pain
It is not unusual for you to get increased pain or altered sensation for a few days to a few weeks after surgery as your spinal cord and/or nerves recover from your surgery. It is important that you stay mobile and continue with your physiotherapy exercises following discharge. Some patients may experience a flare up of symptoms/pain approx. 1-2 weeks after surgery, this usually settles over time, but it is not unusual to get fluctuations in pain/symptoms over many weeks/months. Nerve recovery can take up to 2 years and patients will often see improvement in their symptoms up to this time. Therefore, patience is key!
Activity
It is important to keep mobile after surgery, you will find you get stiff if you sit for more than 20 minutes. You should progressively return to your normal daily routine as quickly as possible.
Remember that you have had an operation and it is usual to feel tired after this. Pace yourself and gradually build up your level of activity. Doing small things often, rather than all in one go is more sensible.
You can undertake all the usual activities of daily life as you feel comfortable this includes walking, shopping, driving and sexual activity.
Research has shown that patients who return to normal routine as quickly as possible make the best recovery. You should progressively return to your normal daily routine as you continue to recover.
Surgical stockings
You should wear your surgical stockings for up to 6 weeks post-surgery, if your mobility is restricted or 2 weeks if you are fully mobile to reduce the risk of DVT (blood clots in the legs).
Follow up
You will be sent an outpatient appointment for approximately 3 months following surgery by post to either come for a face to face appointment or in some cases by telephone. Here you will be seen/spoken to by either a doctor or a nurse specialist. You will usually require x rays at this time.
Concerns
If you have any queries then please do not hesitate to contact the spinal nurses on the advice line 0151 556 3424. Please leave your name and telephone number clearly on the answer machine so we can call you back. We try to answer the messages every working day. We work Mon- Fri 8am-6pm, we do not work weekends. We do spend a lot of time on the wards and in the out-patient clinics seeing patients, so please be patient, we will call as soon as we can.
Physiotherapy
This information is intended to answer the most commonly asked questions. Any further enquiries can be directed to the Physiotherapy department.
General advice
It is safe to continue with all regular activities such as cooking, cleaning, shopping and sexual activity.
You can sleep in whatever position is easiest for you.
You may continue to have some back/leg discomfort or changes in sensation especially for the first 12 weeks, this is normal.
There is no evidence to say that returning to activity and exercise leads to any adverse effects or the need for re-operation.
Driving
You can drive when you can have a full range of movement and you must have full movement to allow you to have full control of the car, this includes being able to do an emergency stop. This is usually a few weeks after surgery.
Work
You can return to work when you feel able and this can depend on what your job role involves. People who return to work sooner have been shown to have better outcomes. You can return to work as soon as you feel you can cope, even if your back is still uncomfortable. Those with desk based roles may feel comfortable to return to work 6 weeks post surgery, but would need to be able to get up and move around to prevent stiffening in the back area. Those with more manual jobs may need to wait the full 3 months before being able to return. You may wish to go back to work as a phased return, please discuss this with your nurse specialist or medical team if you are unsure. It is normal to feel tired when returning to work after a period of sickness absence. You should plan to pace yourself and take regular breaks.
Travel
Generally, we advise not to fly short haul for 6 weeks and long haul for 3 month post surgery, due to the risk of DVT.
Lifting
There is no restriction in bending forwards to pick up light objects or putting on your shoes and socks. Heavy lifting should only be performed in the correct way and should be avoided for the first three months. You can resume lifting when you feel able to do so. There is no given weight we advise as everyone has their own usual capabilities. You can gradually increase the amount you do until you are back to your typical ability.
Exercise
General activity and exercise has been shown to be safe and beneficial for your overall health. We have included an exercise programme however general activities that you may already enjoy have been proven to be as effective therefore you should look to gradually resume these. For example, hiking, swimming, cycling, jogging, yoga and Pilates. Keeping a record/ diary may help you in guiding your progression. Some discomfort is normal when re-commencing activity; you should work within reasonable limits. You should aim to keep your activity low impact for three months after your operation.
You can also safely return to recreational sports such as football or golf in a gradual manner, generally after 3 months. For specific advice with regards to contact sports/ extremes of exercise this should be discussed with your medical team.
Exercise Programme
Aim to do these exercises once per day. These can be started straight away. You can perform them several times per day ensuring that you pace yourself. Start gradually with a low number of each exercise and increase as you are able. These exercises can be complemented by general activity that you enjoy as previously mentioned. It is okay if you miss a day, or have a day off, to let your body rest if you feel this is needed due to expected aches and discomfort.
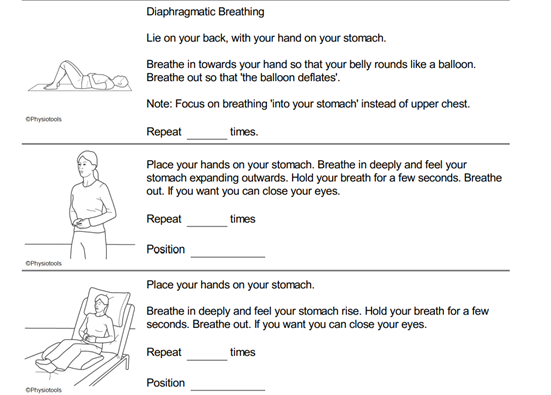
Breathing exercises
Following your surgery you might find that breathing becomes more uncomfortable due to the wound site and procedure. We have enclosed some breathing exercises to help make this easier. We recommend that you complete the exercises provided to help with your recovery. This can be done in a variety of postures, see below. Aim to hold your breath when trying these exercises. Repeat 5 times before taking a break. You can perform them hourly in the first days post surgery.

In a seated position, whilst maintaining your bottom in contact with the seat, gentle lean forward arching the middle of your spine to look at feet. Return slowly to the start position.

In a seated position facing a wall (or appropriate alternative); whilst maintaining your bottom in contact with the seat, reach forward with one arm to touch a point on the wall. Repeat with alternative arms.
(You should feel a gentle stretch in your spine on reaching forward; care should be taken to not reach too far forward that you lose your balance)

In a seated position; with a table in front; place a cloth (or frictionless alternative) on the table. Practice with your left hand moving the cloth from the bottom left hand corner of the table to the top right hand corner of the table. Change hands and repeat.

In a seated position, place a small item (e.g. a cup, tall glass or drinks bottle) on the floor at the side of the front leg of the chair; whilst maintaining your bottom in contact with the seat; practice reaching down to pick up the cup then place it back onto the floor. Repeat this with the other arm.

In sitting on a bed; initially facing forward, place both hands by the side of one leg. Slowly walk your hands around your back until you feel a gentle stretch in your back. Repeat to the other side.

In sitting, fold your arms in front of you; gently turn to one side (aiming to look as far over one shoulder as you can); rotating you spine to feel a gentle stretch.
Twist all the way to the right side and then to the left.

On all fours on the bed, arch your back whilst tucking your head down.

In lying on your back; whilst maintain your hips and legs straight in the bed; raise your arms up in front of you and rotate them across your body, over to the right and then to the left.

In lying on your back; whilst maintaining your shoulders in contact with the bed; raise one knee (maintaining your foot in contact with the bed). Slowly move your knee over to the opposite side, rotating your hips.
Repeat to the opposite side.
Glossary
MRI scan
This is a scan that uses the magnetic fields of the cells in the body. It can provide very detailed images of both head and spinal structures. It requires the person having the scan to lie still in the scan tube for approximately 30mins. Any movement can distort the final images so it is very important to remain completely still for this type of scan.
CT scan
This type of scan is useful for giving accurate pictures of the structures within the spine, especially detail of the bony structure. It uses x rays in a particular way to form the pictures.
Spondylosis
Degenerative changes in the joints of the spinal column, usually as a result of osteoarthritis.
Radiculopathy
This is the name given to problems, for example pain or weakness, that occur as a result of pressure on a particular individual spinal nerve root (rather than multiple different nerve roots).
Disc degeneration
Wear and tear of the disc in between the vertebrae.
Stenosis
Spinal stenosis is when the spinal canal is too narrow and the spinal cord/nerves become too tight in the narrowed space. This can be due to congenital narrowing or degenerative changes. A laminectomy (see next page) is often performed to give the spinal cord/nerves more space.
Osteophyte
This is a bone spur. These bones projections form along joints and occur naturally in the spine as a person ages. They often only cause a problem if they cause any pressure on the spinal cord and/or nerves.
References
BASS Scoliosis https://spinesurgeons.ac.uk/resources/Documents/Booklets/(FINAL)%2000537-22%20Degenerative%20Scoliosis%20Surgical%20Options.pdf
Royal College of Anaesthetists – Preparing for Surgery, Fitter Better Sooner on https://rcoa.ac.uk/sites/default/files/documents/2022-10/FitterBetterSooner2022web.pdf
- Last Updated:01 March 2023
- Review Date:01 March 2025
- Author:Elizabeth Young
- Summary:
This booklet contains information about thoracic spine surgery. There is an explanation of some terms that you may hear. If you have any questions before or after your surgery, then please contact us via the contact details below.