Ventriculo-Peritoneal Shunt Post operative Information
What is a Ventriculo-Peritoneal (VP) shunt?
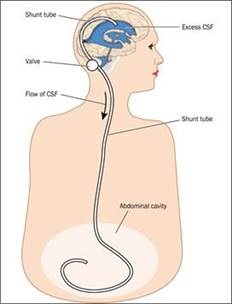
This is a device which diverts the fluid which surrounds the brain and spine (CSF). It consists of a series of tubes with a valve to control the rate of drainage and prevent back flow. It is inserted under general anaesthetic. The upper end is in the ventricle of the brain and the lower end drains into the abdomen (peritoneum). The fluid that is drained, is absorbed into the bloodstream. It is completely enclosed within the body.
How long should it take for me to get over my surgery?
This depends upon a number of things:
- How unwell you were before your surgery.
- Your general health, and if you have any other medical conditions.
- If there have been any complications from your existing medical conditions or your surgery.
There are lots of things which can affect how long it will take for you to get over your surgery, so it is impossible to give an exact timescale.
Your body is unique, so it is important to remember that different people recover at different rates. If your surgery was straightforward the recovery period can be divided into two periods: up to three months after surgery, and three months onwards.
The first twelve weeks
During this time you will experience the most recovery. Initially you may feel tired, and it is important to remember that whilst you have been in hospital you will have been assisted with daily tasks. You may be surprised at how tired you feel once you are at home. The important thing is that you listen to your body; it will guide you as to how much you are able to do. It is not uncommon to need a rest during the day, although this tiredness will gradually improve. After about three to six weeks you should feel stronger and be able to carry out more of your normal activities. You may find your concentration and memory problems persist for a while after surgery this may slowly resolve and again will affect different people in varying degrees.
At about six weeks post surgery you can return to work. It may be advisable to return part time, if you feel this is necessary, as you gradually return to normal. This can be discussed with your Specialist Nurse. It is important that you increase your exercise and tasks gradually, so as not to lose your confidence. Remember, some people are able to do things more quickly than others, and there is no right or wrong for how long it takes to improve.
When will I see my consultant?
Your outpatient appointment will be sent to you through the post, normally for 10-12 weeks post-operatively. An official discharge letter will be sent to your GP after you are discharged. At your follow up appointment you will see a member of your consultant’s team, who you will have met during your admission.
Your general progress will be reviewed and further plans for review will be made with you. At this point in your recovery, you should be back to your normal level of activity.
Eye care
If you have had problems with your vision, you may have seen an eye specialist (ophthalmologist) whilst you were in the Walton Centre. If so, you will be followed up in a separate clinic. If your vision is not affected, it is advisable that you see your own optician every 12 months, and have an eye examination. This will keep a check on the small vessels behind your eyes.
Medicines
If you have been prescribed any new medication during your admission, discuss their continued use with your GP. DO NOT STOP taking them without medical advice.
If you have been prescribed painkillers, and no longer have pain, then you should stop these, again after seeking medical advice. This can be given by your GP.
Programmable shunt valves
Your team will let you know if you have a programmable valve in situ. These can be altered by large magnets such as MRI. Please let the scan department know if you have a programmable valve in situ.
Care of your wounds
Following your discharge from hospital, it is important to keep your wounds clean, dry and covered. You will be given spare dressings to take home by the ward staff. You do not need to change your dressings unless they become loose and are not sealed all of the way around.
This is to reduce the risk of introducing infection to your wounds.
The dressings used are waterproof, so you can shower once home. It is advisable to shower rather than have a bath if possible until your wounds are fully healed, and your stitches or clips are removed.
The stitches/ clips to your head and neck wounds (if you have both) will come out at seven days post surgery,( if it was your first operation) and 10 days for your stomach wound.
If it a repeat operation, the stitches/clips may stay in slightly longer, at 10 days for your head and neck, and 14 days for your stomach.
You may be asked to go to a Walk In Centre or to your practice nurse to have your stitches/ clips removed. If you have had problems with your wound, you may be asked to return to clinic to have your stitches/clips removed and your wound reviewed.
What is normal?
Your head
You may have some swelling over your wound site. This is often just a collection of fluid which will gradually disappear, this is often slightly worse in the morning, improving as the day goes on. As this subsides you may be able to feel the valve of your shunt behind your ear. You may, if you are thin, be able to feel the tubing from the shunt in your neck. This is all normal.
Your stomach
Your wound may be sore for up to a week after your operation, although it is important that you keep mobile. You may notice some numbness around your wound. This is normal, due to the small nerves in your skin being cut during the surgery. You may also have some altered sensation (feeling) around your wound, often described as shooting pain. Your wound may also become itchy as it heals.
Seizures (fits)
These can occur in anyone who has a shunt. The risk of having a seizure is small in normal circumstances. Your consultant will explain more if you need further information.
Alcohol
A glass of wine, or similar, in moderation is acceptable. You must remember that the effects of any medicines you may be taking may be altered by alcohol.
Headache
These vary from patient to patient. Some have little in the way of headache, whilst others find them more troublesome. You should take your prescribed pain medicine regularly. It is not advisable to take pain medicine, bought at the chemist, or supermarket, if not prescribed by your GP or Consultant. If you suffer with headaches after your surgery, it is important to drink plenty of non-fizzy drinks, as dehydration can make headache worse.
It may take longer for the headache to resolve than the standard recovery time. This can be discussed further with your consultant or Nurse Specialist.
Posture can have an effect after your surgery. If you sit or stand up too quickly, you may feel dizzy or get a headache. If this persists and is affecting your ability to walk around, contact your consultant secretary or your Specialist Nurse.
How long should it take for me to get over my surgery?
Exercise
Walking and gentle exercise can be done almost immediately, when you feel up to it.
It is advisable to avoid any contact sports, until you have seen your consultant’s team at 6-12 weeks after your surgery, to avoid any blows to the head or neck. From 6 weeks onwards, non-contact sports can be resumed, and you can return to the gym. Avoid lifting weights which may put strain on your neck.
Most people can resume contact sports after a period of about six months post surgery. Swimming can be resumed once all of your stitches/clips are removed and your wounds are healed. Take a friend for company on your first few swims!
The important points to remember are to do as much as is comfortable, it is important to stay active but avoid overtiring yourself.
Mobile Phones
Evidence suggests there is minimal risk to your shunt from a modern mobile phone.
Hair care
You will have had your hair washed whilst you were in hospital using an antibacterial shampoo. You can wash your hair at home 24hours after your stitches/clips have been removed. This allows the small holes caused by these items to heal.
You can go to the hairdressers to have your hair cut. Inform them that you may be tender over your shunt site.
It may be uncomfortable to have your hair washed over a traditional hairdresser’s sink, and it is not advisable to overstretch your neck. They can wash your hair using a different method if you request it. You may colour your hair 4 weeks after your surgery. Remember your scalp may be more sensitive over your scar.
Travel
If you have holidays planned, discuss this with your consultant’s team.
If you need confirmation you are fit to travel, your consultant’s team can issue this.
You must ensure your travel insurance is updated BEFORE you travel, and that the medical department of your insurance company is aware you have had a shunt inserted. If you have a programmable shunt (your consultant’s team will let you know) you should not go through the magnetic metal detector at the airport. This depends upon the manufacturer of the shunt. A letter to inform the airport security can be issued by your team for you to take with you, as evidence that you have a shunt in place if required.
You can travel by train or coach with no restrictions.
Driving
You will need to let the DVLA know that you have had a new shunt fitted or the upper part of it changed (the ventricular catheter). The legal requirement following either of these types of surgery, is not to drive for six months. The forms to notify the DVLA are available in print, in English, Welsh and other languages from the specialist nurse, or you can download them at home from www.dvla.gov.uk
The DVLA will liaise if necessary with your consultant and let you know in writing when you can return to driving. If you drive without permission from the DVLA, and you are involved in an accident, your insurance will not cover you. The DVLA may request that you have an eye test before they decide if you can drive.
If I have a problem who do I call?
If you have any further questions regarding your shunt, which have not been covered within this information leaflet, or you are concerned please contact: the secretary for your consultant via switchboard on 0151 525 3611, or ask to speak to The Hydrocephalus Nurse Specialist Team on 0151 525 3611 bleep 5340, who will be happy to answer your questions, or general concerns.
If you are unwell, the nurse specialist may arrange for you to attend the Walton Centre for review, advise you to see your GP or to go to your local Accident and Emergency department.
Emergency Access Clinic
Here at The Walton Centre we operate an emergency access clinic for those of our patients who have had a shunt fitted. This clinic is accessed via the Hydrocephalus Nurse Specialist Team, referral via contact through the bleep or through your GP. If you have been treated previously at the Walton Centre you will have access to this clinic.
This clinic runs weekdays and you will be seen by the Nurse Specialist team, assessed, any investigations requested and reviewed by the medical team and further treatment or follow up arranged as appropriate.
What is important for me to tell my doctor?
If you are concerned about the function of your shunt and have any of the symptoms listed below during daytime office hours, you should contact the Nurse Specialists on 0151 525 3611 bleep 5340.
Out of hours contact your GP or go directly to your local A & E.
Wound
- Increased redness
- Swelling around or below the wound
- Leakage of fluid
- Discharge
- Visible shunt tubing through any of your wounds
Headaches
- Increasing in severity, not helped by your normal painkillers
Increased
- New visual disturbances
- Problems with speech
- Drowsiness
- Confusion
- Weakness
- Seizures
- Falls
If you see your GP or attend Accident and Emergency, the doctor can contact a member of the on-call neurosurgical team 24hrs a day, through the switchboard, for advice if required.
If you develop any of the symptoms listed below you should call 999 and go directly to your local A+E:
- Drowsiness to the point where you cannot have a conversation
- Headache accompanied by nausea (feeling sick) and vomiting (being sick)
- Seizures (fits) new or increasing in frequency.
Fever, sweats, neck stiffness or intolerance to light (photophobia)
- Pain or swelling to your legs / calf
- Chest pain or shortness of breath. The advice given in this leaflet does not replace a medical consultation. If you are concerned about your shunt please contact one of your consultant’s team, or seek medical advice.
- Last Updated:01 May 2022
- Review Date:01 May 2025
- Author:Sara Kewin
- Summary:
This is a device which diverts the fluid which surrounds the brain and spine (CSF). It consists of a series of tubes with a valve to control the rate of drainage and prevent back flow. It is inserted under general anaesthetic. The upper end is in the ventricle of the brain and the lower end drains into the abdomen (peritoneum). The fluid that is drained, is absorbed into the bloodstream. It is completely enclosed within the body.