Vertebral compression fracture (VCF): Vertebroplasty and Kyphoplasty
Following your recent investigations and consultation with the spinal team, your scans have revealed that you have one or more fractured vertebrae. This may of been caused by a number of things osteoporosis, traumatic injury to your back or less commonly cancer, as these can all weaken a bone’s structure.
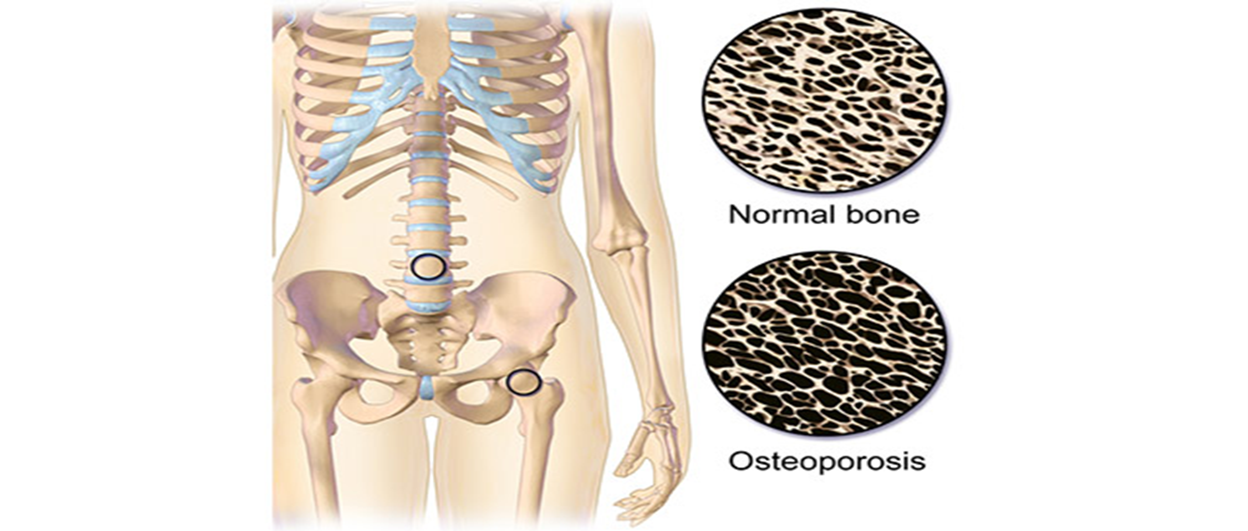
Osteoporosis is a health condition that weakens the bone and becomes more fragile. This then results in a loss of normal bone density, mass and strength, which can result in the bones becoming more susceptible to breaking.
Many other factors can also increase the risk of developing osteoporosis, including:
- Women during/ after menopause.
- High-dose steroid tablets for more than 3 months.
- Long-term use of certain medicines that can affect bone strength or hormone levels.
- Inflammatory conditions, hormone-related conditions, or malabsorption problems.
- Family history of osteoporosis.
- Previous/ current history of an eating disorder such as anorexia or bulimia.
- Low body mass index (BMI).
- Lifestyle such as lack of regular exercise, heavy drinking and smoking.

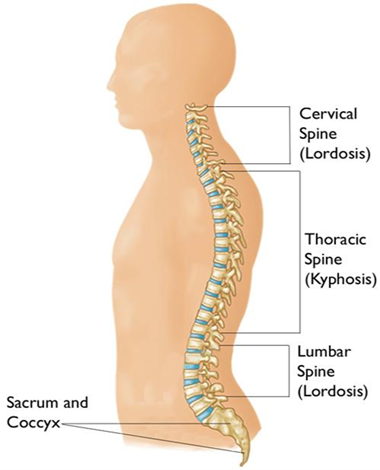
When a vertebral body fractures, the bone squashes down (compresses) and the usual rectangular shape is permanently altered. Typically, this occurs at the front edge of the vertebra (anterior column) and will give the bone a wedge like appearance (anterior wedge compression fracture).
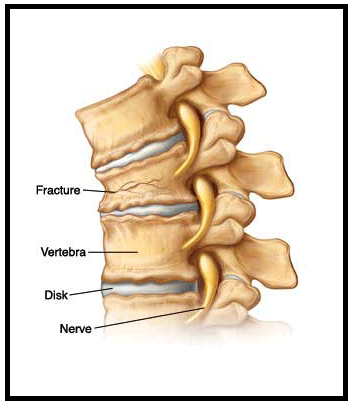
This type of fracture of the vertebral bone can cause extreme back pain along with other symptoms, such as losing height, spinal deformity or a ‘hunched’ appearance (kyphosis) because of the increased forward tilt of the spine. These appearances can be more pronounced the more bones that are involved
Vertebroplasty and kyphoplasty are surgical procedures where bone cement is injected into a fractured vertebrae to stabilise it and reduce the pain. Vertebral body compression fractures are usually treated by conservative measures, such as strong medication, bed rest and/or bracing until the pain settles. Vertebroplasty or kyphoplasty can now be offered to patients where these treatments have been difficult to tolerate and for patients who:
- Incapacitating pain.
- Conditions that limit ability to tolerate bed rest or the taking of strong medication.
- Elderly or frail and are likely to have impaired bone healing following a fracture.
- Vertebral compression fracture due to a malignant tumour.
- Osteoporosis due to long-term steroid treatment or a metabolic disorder.
There are, however, limitations to what this type of treatment can achieve. As some of the pain may also be due to muscular spasms resulting from the spinal deformity. This can be common following an injury, as by adopting a change of posture by leaning backwards to try and ‘reverse’ the forward tilt (thoracic kyphosis) of the spine. This can increase the load on the joints, resulting in inflammation and pain.
The Procedure
Your doctor may advise you to stop taking aspirin, non-steroidal /anti-inflammatory drugs (NSAIDs) or blood thinners several days prior to your procedure.
- The procedure can be carried out under both local or general anaesthesia.
- You will lie prone (lying on your stomach).
- The treatment area of your back will be cleaned, shaved and numbed. Using antiseptic solution and a small incision is made to one or both sides of the midline (centre).
- There will be a small incision for each vertebra requiring treatment.
- A hollow needle is then passed down through the muscle into a bony passage (pedicle)
- X-ray is used as guidance to direct the needle into this area.
- You may feel a tapping sensation during the procedure as the trocar is advanced into the bone.
- Several X-rays may be taken taken from the side and back views, to ensure that the needle is through the pedicle and into the vertebra.
For vertebroplasty, the liquid cement is injected into the vertebra through the hollow needle. Several x-rays are taken to show the cements movement into the vertebra. The cement becomes hard in minutes.
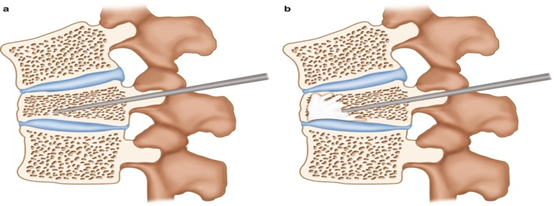
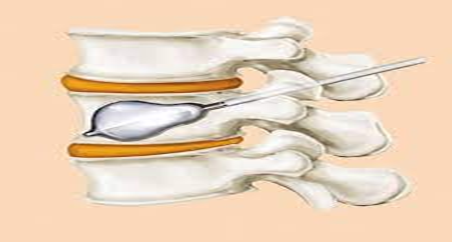
For kyphoplasty, a balloon is first inserted into the fractured vertebrae through the hollow needle to create a cavity or space. The balloon is then removed and the liquid cement is injected into the cavity it created. Several X-rays are taken to show the cements movement into the vertebra. The cement becomes hard in minutes.
Post Procedure
There will be no restrictions with mobility unless the spinal team tells you otherwise. In a majority these are done as a day case procedure.
You will be advised to increase your activity gradually and resume all your regular medications. At home, patients may return to their normal daily activities, although strenuous exertion, such as heavy lifting, should be avoided for at least six weeks.
If you take blood thinners, check with your doctor about restarting this medication the day after your procedure.
Pain relief is immediate for some patients. In others, pain is eliminated or reduced within two days. Pain resulting from the procedure will typically diminish within two to three days.
For two or three days afterward, you may feel a bit sore at the point of the needle insertion. You can use an icepack to relieve any discomfort but be sure to protect your skin from the ice with a cloth and ice the area for only 15 minutes per hour. Your bandage should remain in place for 48 hours. Do not immerse the dressing in water for 48 hours. This is to prevent infection. Taking showers is allowed.
The ward nurses will provide a short period of observation and once you are comfortable and the team are happy you are at your baseline you can return home.
Benefits
- Vertebroplasty and kyphoplasty can increase a patient's functional abilities and allow return to the previous level of activity without any form of physical therapy or rehabilitation.
- These procedures are usually successful at alleviating the pain caused by a vertebral compression fracture; many patients feel significant relief almost immediately or within a few days. Many patients become symptom-free.
- Following vertebroplasty, about 75 percent of patients regain lost mobility and become more active, which helps combat osteoporosis. After the procedure, patients who had been immobile can get out of bed, and this can help reduce their risk of pneumonia. Increased activity builds more muscle strength, further encouraging mobility.
- Usually, vertebroplasty and kyphoplasty are safe and effective procedures.
- No surgical incision is necessary—only a small nick in the skin that does not need stitches.
Risks and Complications
As with any form of surgery, there are risks and complications associated with this procedure. These can include:
- Leakage of the cement outside the vertebral body, which could cause thermal (heat) and pressure problems in the spinal canal. This in turn could cause neurological (nerve) problems including, in extreme cases, paralysis. X-rays are taken throughout the procedure to observe for signs of leakage. The surgeon can stop injecting the cement immediately, if this occurs, therefore minimising the risk of nerve damage
- Travelling of particles of cement, air, bone marrow fat or tumour, into the blood vessels causing a blockage (embolisation). This could in extreme cases put stress on the lungs, heart or other organs.
- Cement sensitivity, which could cause the heart to have irregular beats. This could, in extreme cases, bring on a cardiac arrest (the heart to stop) and death.
- Infection. Superficial wound infections may occur in 2–4% of cases (up to 4 out of 100 people). These are often easily treated with a course of antibiotics. Deep wound infections may occur in < 1% of cases (fewer than 1 out of 100 people). These can be more difficult to treat with antibiotics alone and sometimes patients require more surgery to clean out the infected tissue. This risk may increase for people who have diabetes, reduced immune systems or are taking steroids
- Bleeding. You must inform your consultant if you are taking tablets used to thin the blood, such as warfarin, aspirin, apixaban, rivaroxaban or clopidogrel. It is likely you will need to stop taking them before your operation as they increase the risk of bleeding. If your operation is scheduled with less than a week’s notice, please check with your consultant or nurse which drugs need to be stopped to prevent your surgery being delayed.
- The increased strength in the vertebra following vertebroplasty, may increase the chances of the adjacent vertebral body wedging in the future.
- When positioning during the operation which might include pressure problems, skin and nerve injuries and eye complications including, very rarely, blindness. A special gel mattress and protection is used to minimise this.
- Extremely rarely, death; as a result of damage to major blood vessels or vital organs at the front of the spine, which is reported as happening in 1 out of 10,000 cases
- General anaesthetic fatal complications which have been reported in 1 out of 250,000 cases.
Follow Up
Your specialist spinal nurse will advise regarding follow up whether that be virtual or in person. If you have any queries you can contact spinal nursing team on 0151 556 3424.
Osteoporosis Support
The Royal Osteoporosis Society is the UK's national charity for osteoporosis. It has detailed information about osteoporosis prevention and treatment, and support groups throughout the UK.
Find an osteoporosis support group near you on the Royal Osteoporosis Society website. https://theros.org.uk/information-and-support/support-in-your-area/find-your-local-support-group/
The Royal Osteoporosis Society's free telephone helpline may be particularly helpful if you're newly diagnosed with osteoporosis. The helpline number is 0808 800 0035 and is open Monday to Friday, 9am to 12.30pm and 1.30pm to 5.00pm.
Acknowledgement: BASS 2019. British Association of Spine Surgeons (BASS), RCSEng, 38-43 Lincoln's Inn Fields, Holborn, London, WC2A 3PE. Copyright gained.
- Last Updated:20 January 2023
- Review Date:20 January 2025
- Author:Faye Mangan
- Summary:
Following your recent investigations and consultation with the spinal team, your scans have revealed that you have one or more fractured vertebrae. This may of been caused by a number of things osteoporosis, traumatic injury to your back or less commonly cancer, as these can all weaken a bone’s structure.