Pressure ulcer prevention
Pressure ulcer prevention
The purpose of this leaflet is to provide you and your carer information on pressure ulcers (often known as bed sores or pressure sores), how they develop, and how to prevent them. This leaflet is a guide and often your treatment will be more detailed. You may want to discuss this with your nurse.
What is a pressure ulcer?
A pressure ulcer or bed sore is damage that occurs on the skin and underlying tissue, due to a lack of blood and oxygen supply.
Signs of pressure damage may include:
- Pain/burning over a bony area
- Red patches over a bony area of fair skin
- Purple/black patches over bony area of dark skin
- Blisters
- Heat
- Swelling
Are you at risk?
Anyone can get a pressure ulcer particularly people with poor mobility who spend lots of time in bed or in a chair.
People at risk include those with the following health issues:
- Diabetes
- Poor circulation
- Poor appetite
- Serious illness/Major surgery
- Problems with breathing
- Poor diet and not drinking enough
- Spend long periods in a wheelchair or bed
- Underweight/Overweight
- Loss of feeling (sensation) in parts of your body
Moist skin
You may be at increased risk if your skin is too damp, e.g., incontinence. Therefore it is important that skin is kept clean and dry.
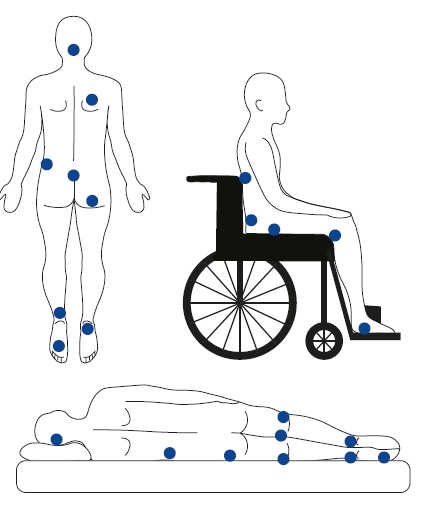
The most common places at risk of pressure damage are the bony parts of your body (marked here in blue)
Be aware that some essential devices can cause pressure damage

How can I prevent pressure damage?
- Assessment - you will be risk assessed on admission to hospital and on each ward transfer.
- Skin Inspection - you will be asked to have your skin inspected at least daily. Please inform the nurse if you have any existing issues.
- Surface - you may need specialist equipment during your stay, mattresses, chairs and cushions. This will be assessed regularly in line with your skin condition.
- Keep moving - it is important to change position as often as possible either by yourself or with help from your nurse.
- Incontinence and moisture - wet skin will damage easily by pressure. Keep skin clean and dry. Barrier creams/films will be supplied if needed.
- Nutrition - Eat a good healthy diet and keep hydrated. A dietician referral will be made if needed.
- Giving information - Please ask your nurse for further guidance on pressure ulcer prevention.
- Last Updated:01 August 2023
- Review Date:01 August 2026
- Author:Jeanette King
- Summary:
The purpose of this leaflet is to provide you and your carer information on pressure ulcers (often known as bed sores or pressure sores), how they develop, and how to prevent them. This leaflet is a guide and often your treatment will be more detailed. You may want to discuss this with your nurse.